Chronic stress affects brain morphology and functioning: relevance to cancer survivors and chronic pain?
Many patients with chronic pain suffer from stress intolerance, and some patients have developed chronic pain during or following a stressful period or (life) event (e.g. motor vehicle accident, trauma exposure). When chronic pain is present, stress typically worsens the pain (severity). Taken together, stress and chronic pain are closely connected. In this blog post fascinating research findings regarding the effect of chronic stress on the brain are presented, providing a neuroscientific explanation why chronic stress may lead to the development of chronic pain.
At least 3 major brain areas are affected by chronic stress: the amygdala, prefrontal cortex and hippocampus. Remarkably, the effects of chronic stress are site-specific: hypertrophy in the amygdale and atrophy in the prefrontal cortex and hippocampus (figures 1 & 2). Such observations were done initially in experimental animal studies, but since then backed-up by human (most often observational) studies (Radley et al. 2015; Vyas et al. 2002). Even within each of the mentioned brain areas, (slight) differences in morphological responses to chronic stress may occur (e.g. amygdaloid hypertrophy is preferentially seen in the basolateral complex of the amygdala). ‘Brain atrophy’ includes neuronal changes, such as reduced dendritic length and branching, decreases in spine density, reduced brain region volume, etc. ‘Brain atrophy’ is thought to be mediated by several factors including high levels of glucocorticoids in response to long-term stress exposure.
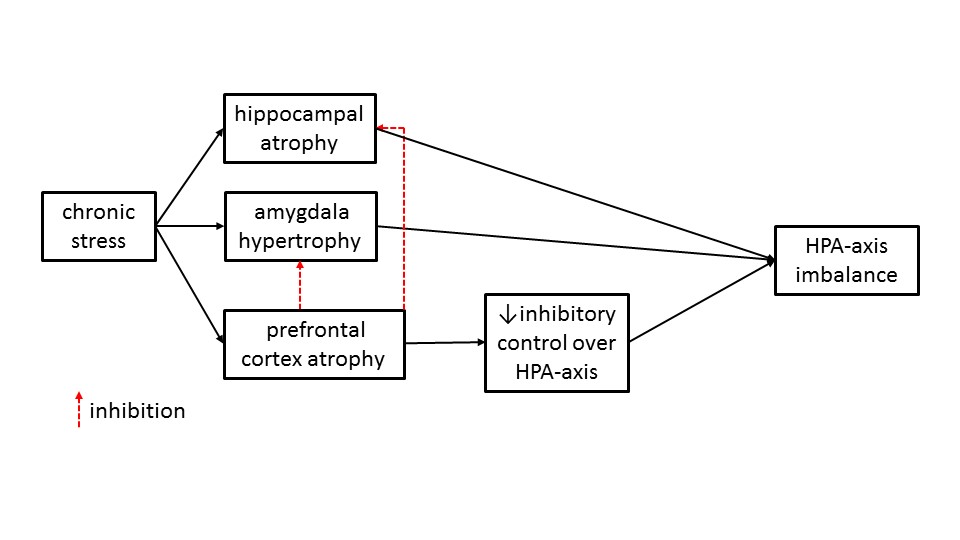
Figure 1: Effects of chronic stress on the hippocampal and amygdala morphology and functioning.
And what do these brain changes imply? Does it has a meaning? Certainly they are not epiphenomena: hippocampal atrophy explains neurocognitive impairments as often seen in chronic pain patients, including impaired memory and so-called ‘brain fog’. Amygdala hypertrophy explains enhanced fear conditioning, abnormally high fear responses and also the development or sustainment of chronic (widespread) pain. Indeed, the amygdala are one of the key brain areas held responsible for the (development of the) mechanisms underlying central sensitization.
Figures 1 and 2 also highlight the important role of all 3 brain regions in top-down controlling of the hypothalamus-pituitary-adrenal axis (HPA-axis), one of the body’s major and crucial stress response systems. The HPA-axis is of cardinal importance for changing energy demands during and following (recovery!) stress (including physical stress and exercise). The hippocampus normally exerts a negative feedback regulation on the HPA-axis, while the amygdala typically activates the HPA-axis. Chronic stress-induced hippocampal atrophy and amygdaloid hypertrophy implies loss of the hippocampal inhibitory control and gain in the amygdala excitatory control over the HPA-axis, respectively (figure 1). Together, these brain changes may explain HPA-axis imbalance as often seen in people with a long period of stress (e.g. patients with post-traumatic stress disorder or some post-cancer patients).
Comparing the impact of the amygdala changes with those seen in the hippocampus, scientists conclude that chronic stress may have a more powerful effect on the amygdala, possibly overriding those seen in the hippocampus. Still, probably the most significant brain area in terms of chronic stress is the prefrontal cortex. Indeed, prefrontal cortex atrophy implies loss of its (physiological) inhibitory control over both amygdala and hippocampus, as well as loss of top-down inhibitory control of the HPA-axis (figure 2). Thus, prefrontal cortex atrophy is another reason why the HPA-axis gets out of control in many (pain) patients exposed to long periods of severe stress.
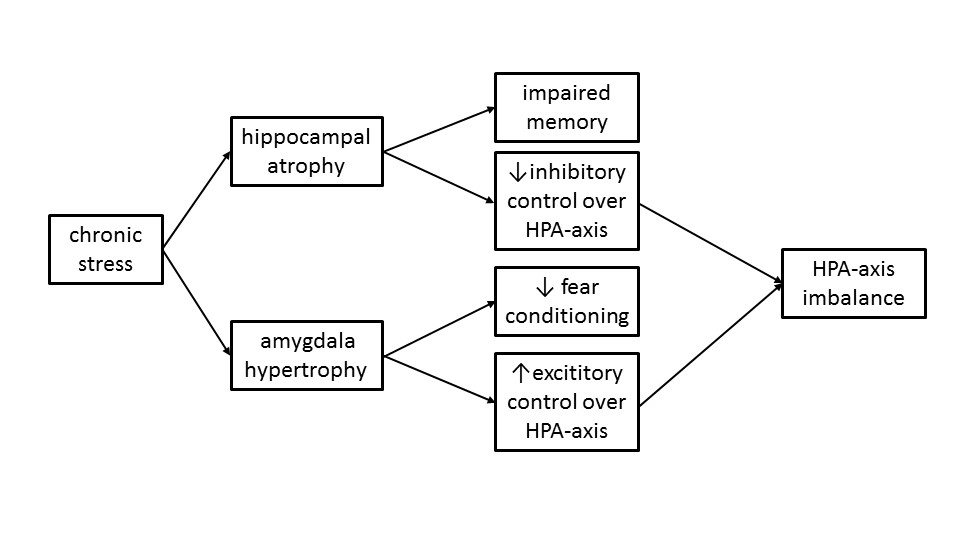
Figure 2: Effects of chronic stress on the prefrontal cortex ability to inhibit the hippocampal, amygdala and HPA-axis.
A final reason why the prefrontal cortex is so significant is because of its therapeutic potential. Exposure treatment and cognitive behavioral-type interventions hold the capacity to target the prefrontal cortex in (pain) patients, and even to restore atrophy. What are we waiting for?
Jo Nijs
2016 Pain in Motion
References and further reading:
Radley J, Morilak D, Viau V, Campeau S. Chronic stress and brain plasticity: Mechanisms underlying adaptive and maladaptive changes and implications for stress-related CNS disorders. Neuroscience and Biobehavioral Reviews 2015; 58:79-91.
http://www.ncbi.nlm.nih.gov/pubmed/26116544
Vyas A, Mitra R, Shankaranarayana Rao BS, Chattarji S. Chronic stress induces contrasting patterns of dendritic remodeling in hippocampal and amygdaloid neurons. Journal of Neuroscience 2002;22(15):6810-8.