Patient’s pain and disability improvement is an everyday challenge for physiotherapists. Often, unexpectedly, the clinical condition of a patient changes along the treatment, worsening or improving without a particular, evident reason. As physiotherapists, we have asked ourselves many times the reason behind this clinical phenomenon that defies our clinical reasoning and undermines our prognostic expectations, based on a well-structured therapeutic plan. We think that most of the answer relies on the fact that the clinical outcome is determined both by the appropriateness of the therapy adopted and by the modality by which it is delivered.
Indeed, several contextual factors (CF) that usually surround the professional encounter between physiotherapist and patient have been demonstrated of having a high clinical impact (FIGURE 1).
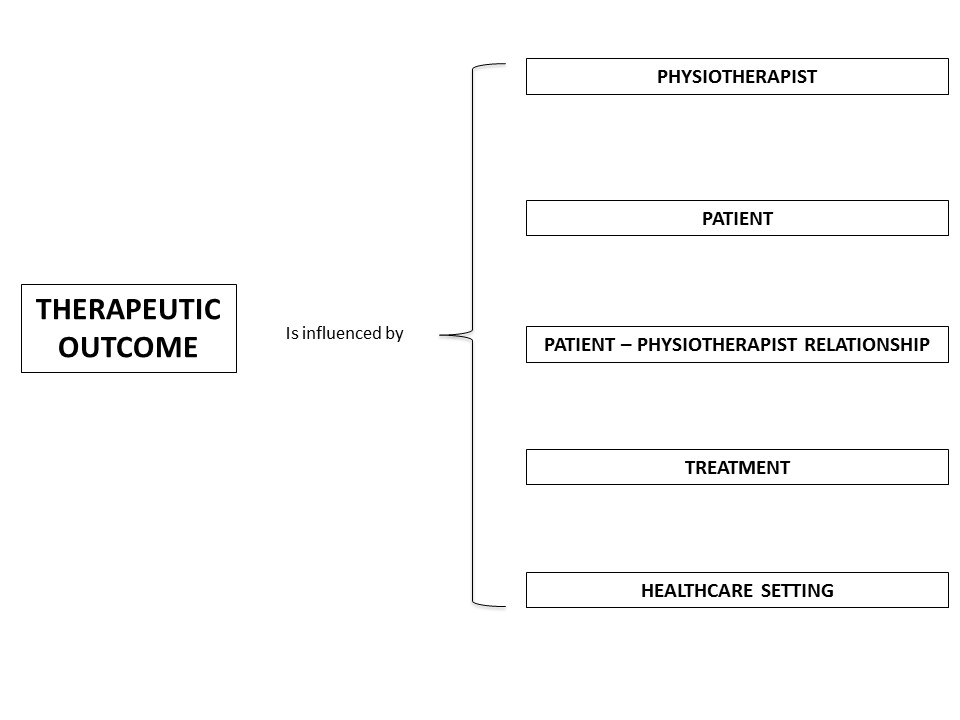
FIGURE 1. The contextual factors relevant for physiotherapy.
Professional behaviour, appearance, beliefs and behaviour of the physiotherapist about the pathology, each can impact the clinical condition of the patient. The patient’s previous experience, preference and expectations are key elements to consider when choosing the treatment. The verbal and non-verbal communication (postures, gestures and touch) is an essential component of the patient-physiotherapist relationship. Providing a clear diagnosis, performing an overt therapy, using an observational learning strategy and the adoption of a patient-centered approach are fundamental elements of an effective global process of care. Also the environment, the architecture and the interior design of the healthcare setting can influence the efficacy of therapy and, when possible, should be used accurately for inpatient and outpatient physiotherapy.
All these factors are capable to modulate the therapeutic outcome generating placebo and nocebo responses able to modify the therapeutic trajectory towards a positive or negative direction and influencing patient’s satisfaction. Different theories, enclosing expectation, learning and conditioning, help to explain the psychological perspective behind placebo, nocebo and context effect. A robust body of knowledge has identified a specific neural network, composed by the anterior cingulate cortex, the dorsolateral prefrontal cortex, the hypothalamus, the periaqueductal gray, the rostro-ventro-medial medulla and the dorsal horn of the spinal cord, that is implicated in pain modulation (FIGURE 2). This can be considered the neurophysiological aspect supporting the clinical changes induced by the contextual factors throughout placebo and nocebo effects.
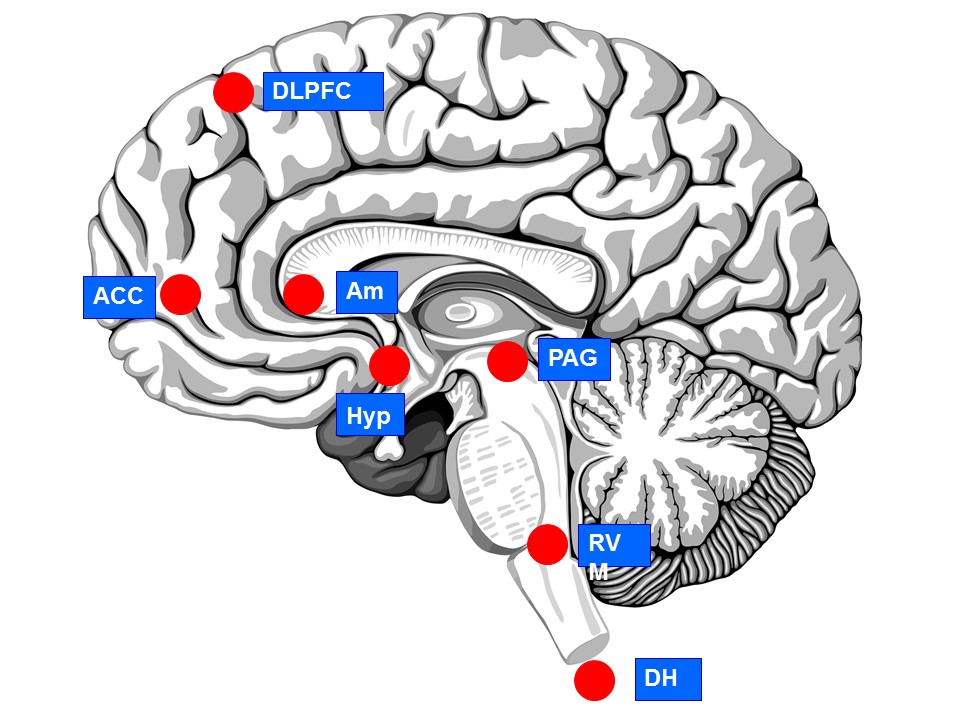
FIGURE 2. The neural network behind contextual factors effect.
DLPFC, dorso lateral pre frontal cortex; ACC, anterior cingulate cortex; Am, amygdala; Hyp, hypothalamus; PAG; periaqueductal gray; RVM, rostral ventromedial medulla, DH, dorsal horn of spinal cord.
The good news is that a patient’s clinical condition can be influenced by contextual factors. The bad news is related to the complexity, some uncertainty and risk for patient’s deception behind their use. Nevertheless, physiotherapists have already enough scientific information that allows them to adopt correct behaviours and modify the contextual factors around the therapy in an evidence-based and ethically respectful perspective.
Future studies should assess the actual weight of the contextual factors on the quality of the therapeutic outcome by clinical controlled trials comparing usual therapy with therapy enriched by specific contextual factors.
Marco Testa & Giacomo Rossettini
2017 Pain in Motion
References and further reading:
Testa M, Rossettini G. Enhance placebo, avoid nocebo: How contextual factors affect physiotherapy outcomes. Man Ther. 2016 Aug;24:65-74.
https://www.ncbi.nlm.nih.gov/pubmed/27133031
O'Sullivan P, Caneiro JP, O'Keeffe M, O'Sullivan K. Unraveling the Complexity of Low Back Pain. J Orthop Sports Phys Ther. 2016 Nov;46(11):932-937.
https://www.ncbi.nlm.nih.gov/pubmed/27802794
Bishop MD, Torres-Cueco R, Gay CW, Lluch-Girbés E, Beneciuk JM, Bialosky JE. What effect can manual therapy have on a patient's pain experience? Pain Manag. 2015;5(6):455-64.