The effect of exercise therapy has been extensively studied in health and disease. While it is broadly agreed that a programof exercisesis beneficial, the same cannot be said for a single session.Symptoms worsening following exercise is indeed a common feature in people with chronic pain.
To understand this unwanted response to physical activity, research has focused on exercise intensity. Investigators manipulated exercise intensity and assessed whether different intensities determined different effects on people’s symptoms or neuro-physiological measures (e.g. pressure pain thresholds (PPTs)).
Exercise intensity can be relevant for some parameters. For instance, exercise-induced oxidative stress increase depends – among other things - on it. However, when it comes to clinical outcomes, responses vary from subject to subject, and exercise intensity does not appear to play a big role. This seems true for healthy subjects as well as for patients. Our group performed a study on healthy sedentary people and patients with chronic fatigue syndrome (Van Oosterwijck et al. 2010). The two groups performed both a submaximal exercise test and a self-paced, physiologically limited bout of exercise, the latter specifically designed to reduce physical stress at a minimum.
Exercise had a beneficial effect on healthy subjects, increasing PPTs, and a negative one on patients, worsening their symptoms. However, within each group, the intensity of exercise did not influence symptoms responses nor PPTs.
But if it is not the intensity of physical activity, what can explain exercise-induced symptom worsening (or relieve)?
Chronic pain patients can perceive exercise as threatening
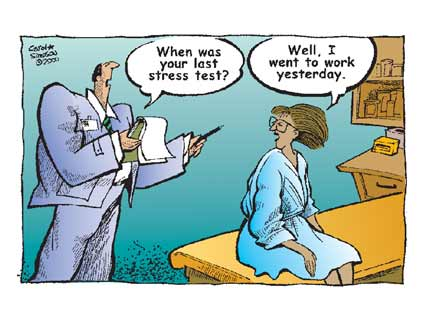
I believe that an underexplored topic in the exercise literature is the relation between the effect of exercise and how the exercise itself is perceived by the subject – especially when it is perceived as threatening or at least stressful by the subject. The idea is that exercise would have positive effects when it is perceived as safe and beneficial, and negative consequences any time it is feared or uncontrollable.
Numerous animal studies from the stress literature offer interesting insights on this. If you are a rodent (hello rodents in the audience!) and you voluntarily choose to run on your wheel, this will reduce stress and improve health. On the contrary, if you are forced to exercise, even though the amount of physical activity is the same, effects can be detrimental (Svensson et al. 2016). In humans, a minor increase (10%) in exercise intensity beyond the level that the subjects would choose for themselves can significantly reduce pleasantness, with no additional gains (Lind et al. 2008). Crucially, increasing perceived control alleviates stress and increases activity (Bhanji et al. 2014).
This evidence can be easily transferred to our clinical practice: any exercise or activity can potentially be perceived as harmful. We need to assess this with our patients, and re-conceptualise what we propose in order to improve perceived control and reduce threat. Exercise should be presented as safe, enjoyable, and controllable, rather than “something needed to improve your health or pain”.
To close the loop, let’s go back to the work from our group I introduced above (Van Oosterwijck et al. 2010). One question remains. The second bout of exercise was specifically designed to reduce threat and increase safety. However, apparently in contradiction with what stated above, it did fail to improve patients’ symptoms – actually worsening them. So, why this? I reckon a possible explanation is that people with chronic fatigue syndrome are arguably the people that fear physical activity the most (and have all the rights to do so, by the way). It is reasonable to think thatexercise itself– even low-demanding ones –can be perceived as harmful, making exercise prescription more difficult.
More research trying to falsify this hypothesis is clearly needed, but to date available literature seems to support the idea that how an activity is perceived can change the effects that that same activity has. I believe this is something we cannot not consider in our clinical practice.
On the quest for mechanisms
A mechanism-based reasoning should always accompany clinical ones. A number of mechanisms might explain how a perceived threatening or stressful event can have negative effects. Threatening situations might lead to significant cortisol hormone increase through the HPA axis, and catecholamine release through the autonomic nervous system. All together, these can promote immune cells activation, and the subsequent increase of inflammation (O'Donovan et al. 2013). Similarly, elevated level of cortisol and noradrenaline promotes glial cells activation in brain regions such as prefrontal cortex, amygdala, and hippocampus (Nijs et al. 2017). Finally, glial cells have to be taken into account. Glia are non-neuronal cells that resides in the central nervous system and exert neuro-immune functions. Activated glia release neurotransmitters and pro-inflammatory cytokines and chemokines, and are therefore capable of inducing and maintaining neuro-inflammation and neurons hyper-excitability. Glia can represent an intriguing link between stress, the immune system, and central sensitization (Nijs et al. 2017), and it is exciting to see more and more scientific work focusing on these cells.
Andrea POLLI
Andrea Polli is a physiotherapist and OMT manual therapist. After his bachelor and master degree in rehabilitation of musculoskeletal disorders, he moved from Italy to the UK, to obtain the MSc in Pain: Science & Society at the prestigious King’s College London. He then returned to Italy for a few years, working at the IRCCS San Camillo Hospital, in Venice. He is part of the Pain in Motion group since 2015, where he works as PhD researcher at the Vrije Universiteit Brussel and KU Leuven, exploring the role of epigenetic changes in chronic pain.
2017 Pain in Motion
References and further reading:
Van Oosterwijck, Jessica, et al. "Pain inhibition and postexertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome: an experimental study." Journal of internal medicine 268.3 (2010): 265-278.
https://www.ncbi.nlm.nih.gov/pubmed/20412374
Svensson, Martina, et al. "Forced treadmill exercise can induce stress and increase neuronal damage in a mouse model of global cerebral ischemia." Neurobiology of stress 5 (2016): 8-18.
https://www.ncbi.nlm.nih.gov/pubmed/27981192
Lind, Erik, Panteleimon Ekkekakis, and Spiridoula Vazou. "The Affective Impact of Exercise Intensity That Slightly Exceeds the Preferred Level: 'Pain'for No Additional'Gain'." Journal of Health Psychology 13.4 (2008): 464-468.
https://www.ncbi.nlm.nih.gov/pubmed/18420754
Bhanji, Jamil P., and Mauricio R. Delgado. "Perceived control influences neural responses to setbacks and promotes persistence." Neuron 83.6 (2014): 1369-1375.
https://www.ncbi.nlm.nih.gov/pubmed/25199702
O’Donovan, Aoife, et al. "Exaggerated neurobiological sensitivity to threat as a mechanism linking anxiety with increased risk for diseases of aging." Neuroscience & Biobehavioral Reviews 37.1 (2013): 96-108.
https://www.ncbi.nlm.nih.gov/pubmed/23127296
Nijs, Jo, et al. "Sleep disturbances and severe stress as glial activators: key targets for treating central sensitization in chronic pain patients?" Expert Opinion on Therapeutic Targets 21.8 (2017): 817-826.