The efficacy of Pain Neuroscience Education (PNE), the explanation of pain to patients with (long-term) pain, has been studied since 2002 (Moseley, 2002). Since then, a great number of researchers all over the globe have further studied the value of PNE in a quantitative manner. Recently, multiple reviews have shown that PNE is efficacious for instance for: decreased pain, disability, improved mental health, kinesiophobia and pain catastrophizing (Louw, 2011, Watson, 2019, Wood, 2019). However, this efficacy accounts for PNE when it is combined with other (physiotherapy) treatment modalities, and PNE is more efficacious when the PNE is of longer duration and in a one-on-one setting (Louw, 2011, Watson, 2019, Wood, 2019). So, to conclude: as the Dutch might say: ‘that’s in the pocket!’. We know when this modality works, so let’s use it in this way! Done business. Right?
Well, it isn’t that black and white. As in any treatment modality there are many shades of grey. Especially, when it is a ‘communication-modality’ such as PNE! Therefore, it is important to investigate the process of PNE. What happens during a PNE session? What are crucial elements? What happens when a patient hesitates or disagrees with the explanation? How to deal with that? How do patients reconceptualize their pain, how do we involve stress related factors and what kind of consequences does this have for the patients? And most and foremost: how do we further improve PNE and the implementation into practice? These ‘grey’-questions are perfect questions for qualitative research.
Multiple qualitative research studies, via interviews, have investigated the ‘shades of gray’ of phenomenon of PNE (King 2018, King 2016, Robinson 2015, Wijma, 2018). Summarizing the thick data from studies in a few sentences is difficult and we therefore suggest reading these comprehensive articles. However, they have shown important factors when providing PNE are, for instance: the therapeutic alliance, the intake prior to the PNE, that individual experiences relevance of the PNE, that the PNE is individualized and that the PNE is repeated. Furthermore, most (however not all) patients in these studies reconceptualized their pain and had a different pain experience (King 2018, King 2016, Robinson 2015, Wijma, 2018).
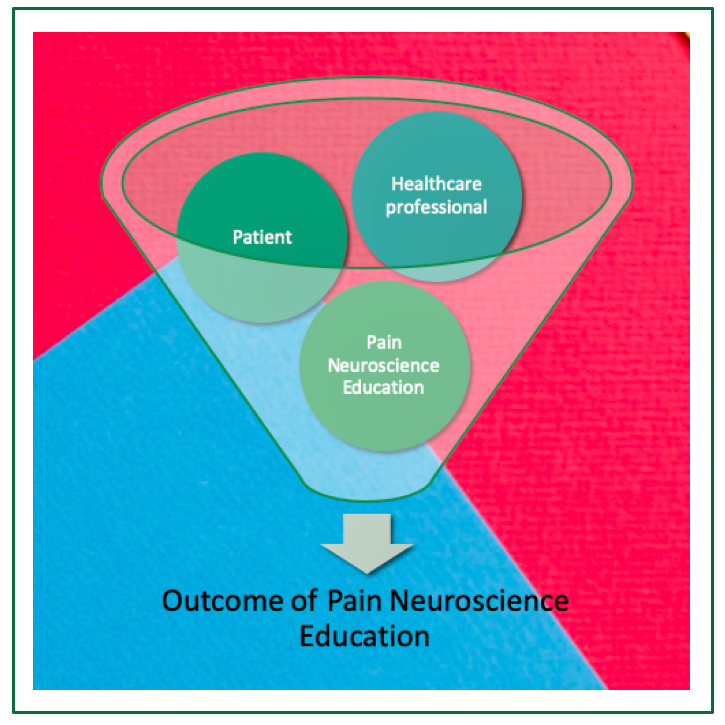
Even though these interviews with patients give us insight in the experience of PNE, it reflects their vision of the experience and not the complete picture of clinical practice. To further understand what happens during the PNE and what the crucial factors in the PNE process are, it is important to use different analysis methods. We therefore conducted a Constructive Grounded Theory study in which the verbal and non-verbal aspects of PNE were investigated. In this study we tried to understand the social processes that happen during the PNE and why some patients agree, while others hesitate or even disagree with the PNE. In order to make PNE more successful, we will theorize this ‘grey area’ and explore which factors are of importance.
We will take you out of the grey when the study is published!
Amarins Wijma
2019 Pain in Motion
References and further reading:
1) Moseley L. Combined physiotherapy and education is efficacious for chronic low back pain Australian journal of physiotherapy. 2002;48(4):297-302. PubMed PMID: 12443524; eng.
2) Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain,disability, anxiety, and stress in chronic musculoskeletal pain. Archives of physical medicine and rehabilitation. 2011;92(12):2041-2056.
3) Wood L, Hendrick PA. A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: Short-and long-term outcomes of pain and disability. Eur J Pain. 2019;23(2):234-249.
4) Watson JA, Ryan CG, Cooper L, et al. Pain neuroscience education for adults with chronic musculoskeletal pain: a mixed-methods systematic review and meta-analysis. The journal of pain: official journal of the American Pain Society. 2019.
5) Louw A, Zimney K, O'Hotto C, et al. The clinical application of teaching people about pain. Physiotherapy theory and practice. 2016 Jul;32(5):385-95. PubMed PMID: 27351903.
6) King R, Robinson V, Elliott-Button HL, et al. Pain Reconceptualisation after Pain Neurophysiology Education in Adults with Chronic Low Back Pain: A Qualitative Study. Pain Res Manag. 2018;2018:3745651.. PubMed PMID: 30275918
7) King R, Robinson V, Ryan CG, et al. An exploration of the extent and nature of reconceptualisation of pain following pain neurophysiology education: A qualitative study of experiences of people with chronic musculoskeletal pain. Patient education and counseling. 2016;99:1389-1393. PubMed PMID: 27021238.
8) Robinson V, King R, Ryan CG, et al. A qualitative exploration of people's experiences of pain neurophysiological education for chronic pain: The importance of relevance for the individual. Manual therapy. 2015 Oct 20. PubMed PMID: 26511524
9) Wijma AJ, Speksnijder CM, Crom-Ottens AF, et al. What is important in transdisciplinary pain neuroscience education? A qualitative study. Disability and rehabilitation. 2018 Sep;40(18):2181-2191. PubMed PMID: 28524700.