Sex differences in pain have been a topic of increased interest in recent years. An expansive body of literature in this area clearly suggests that men and women differ in their response to pain. Controlled laboratory studies have revealed overwhelming evidence for increased pain sensitivity, higher pain ratings and lower pain tolerance of female participants compared with males, although the size of the differences were modest and not always statistically significant (Rosen et al., 2017).
Epidemiological studies reveal prevalence rates of chronic pain in the population that are 6% higher in women versus men. The population prevalence of several common chronic pain conditions is greater for women than men, including fibromyalgia, migraine and chronic tension-type headache, irritable bowel syndrome, temporo-mandibular disorders and interstitial cystitis (Bartley et al., 2013).
The specific underlying mechanisms contributing to this disparity are far from clear. It has been suggested that an interaction of biological, psychological and sociocultural factors likely contribute to these differences.Of the biological explanations, the influence of sex hormones represents a significant source of pain-related variability that likely impacts men and women differently.
The search for mechanisms that contribute to the sex differences in pain led researchers to look at “the other brain”, the immune like cells of the brain and spinal cord, termed Glia. Indeed, in the past decade, it has become increasingly clear that neurons are not the only cell type involved in pain processing in the peripheral and central nervous systems, and that Schwann cells, satellite cells and cells of the immune system such as microglia, macrophages and T-cells are also involved.
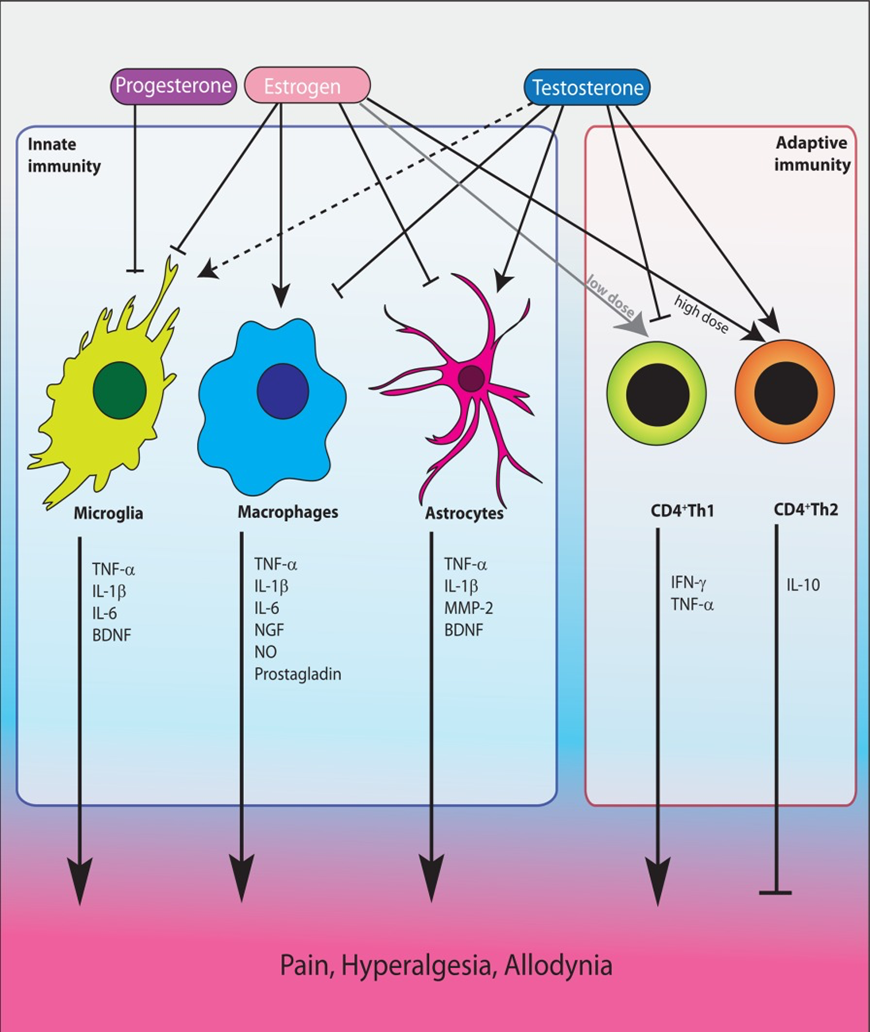
Fig. Effects of gonodal hormones on cells of the innate and adaptive immune system leading to modulation of pain, from Rosen et al.,2017
Given the extensive effects gonodal hormones (see fig) exert on the immune system, it is highly probable that immune cells directly contribute to sex differences in pain. According to Lauren Nicotra (Nicotra, 2013), glia appear to be central to the sex differences in pain. “Female pain is fundamentally different to male pain owing to the different reliance on glia”, she said.
The result is that women’s experience of pain is more severe than men’s and the pain is harder to treat.
The review of Sarah Rosen (Rosen et al.,2017) addresses what is currently known about how immune cells affect pain signaling and chronic pain development and maintenance and how gonodal hormones (estrogens, progesterone and testosterone) affect the immune system.
For researchers, it is vital that all studies in pain research include both sexes in their experiments and analyses. Furthermore, differences between these sexes should be analyzed. Not only will this lead to a more thorough understanding of sex differences in pain, it may also lead to more person-centered targeted therapeutic approaches to treating chronic pain conditions.
Luc Vanderweeen
Master of Science in Spinal Manual Therapy and Physiotherapy
Rug-Schouder-Nekcentrum, Schepdaal, Belgium
Pain in Motion Research Group
2018 Pain in Motion
References and further reading:
Rosen S, Ham B, Mogil JS, Sex differences in neuroimmunity and pain, J Neurosci Res. 2017 Jan 2;95(1-2):500-50
https://www.ncbi.nlm.nih.gov/pubmed/27870397
Bartley EJ, Fillingim RB, Sex differences in pain: a brief review of clinical and experimental findings, Br J Anaesth. 2013 Jul;111(1):52-8
https://www.ncbi.nlm.nih.gov/pubmed/23794645
Lauren Nicotra, https://theconversation.com/women-experience-more-chronic-pain-than-men-now-we-know-why-19648, 2013