At the start of this research series, we were asking the clinical question as to why central sensitisation (CS) develops in some people and not in others. Is it something to do with their personal characteristics of sensitivity? Here, I want to outline what we did to begin investigating this and summarise for you the proposals we came up with.
Our systematic review had shown that pre-morbid sensitivity, using quantitative sensory testing, as well as genetic aspects of sensitivity, were predictive of CS in chronic musculoskeletal pain presentations (J. Clark, Nijs, Yeowell, & Goodwin, 2017). To date, no-one had investigated trait characteristics of sensory sensitivity, trait anxiety and personality types in people with non-specific chronic low back pain (NSCLBP), to see how they related to the extent of CS symptoms.
The aim of this mixed methods study was to identify pre-morbid trait characteristics in people with NSCLBP and CS and to explore their possible role in the development of CS pain.
What we did
We conducted an international cross-sectional observational study using a mixed methods design, with a core quantitative study using questionnaires and a concurrent nested qualitative study using semi-structured interviews. Participants (n = 165) with NSCLBP were all clinically identified as being centrally sensitised. This was done in physiotherapy and pain clinics in New Zealand, England and Ireland using published clinical guidelines for classification of predominant CS pain in people with NSCLBP (J. Nijs et al., 2015; Smart, Blake, Staines, Thacker, & Doody, 2012). We used the Central Sensitisation Inventory (CSI) to measure the extent of CS symptoms, the State-Trait Anxiety Inventory (trait section) with the Marlowe Crowne Social Desirability Scale to identify personality types based on trait-anxiety and defensiveness, and the Adolescent / Adult Sensory Profile (AASP) to identify aspects of sensory sensitivity. The AASP identifies trait sensory hyper-sensitivity with a passive (Sensory Sensitive) or active (Sensation Avoiding) response to over-stimulation; and trait sensory hypo-sensitivity with a passive (Low Registration) or active (Sensation Seeking) response to under-stimulation.
What we found
Results showed that in a NSCLBP population with CS predominant pain:
(J. R. Clark, Nijs, Yeowell, Holmes, & Goodwin, 2019)
It was interesting that the two sensory profiles which predicted CS symptoms were those with a passive adaptive response to sensory discomfort. The more trait anxious, and/or the more extreme the trait sensory processing thresholds, the more central sensitisation symptoms an individual may develop in NSCLBP.
all of which highlighted the context in which CS pain developed. (J. R. Clark, Goodwin, & Yeowell, 2018).
How we interpreted it
Being prone to anxiety, high sensitivity and feeling out of control with passive responses to symptoms, may be part of why some people develop CS. Trauma and high trait anxiety may render a person more sensitive to stressors, leading to physiological arousal. Physiological arousal creates sensations of state anxiety and heightened senses. These in turn may be 1) ignored by the repressor who turns their attention away from them and interprets them in a positive light, or 2) fully attended to and interpreted as threatening by the defensive high anxious individual, who may then become centrally sensitised.
We theorised that the Low Registration sensory profile meant that sensory under-stimulation can be as much of a stressor as sensory over-stimulation. Individuals with developmental learning differences were prevalent in the nested sample, and these are known elsewhere to be associated with sensory processing disorders. Alterations in sensory processing are part of the CS presentation, but the causal link between sensory processing disorders in learning difficulties and those found in CS are unknown, requiring further investigation.
Using the premise that stressors lead to physiological arousal, which is followed by a personality-based response, we developed a proposed pathway to CS. In it is included the need for sleep. Stress, trauma and anxiety are related to poor sleep, which in turn may contribute towards CS (Jo Nijs et al., 2017); (Figure 1).
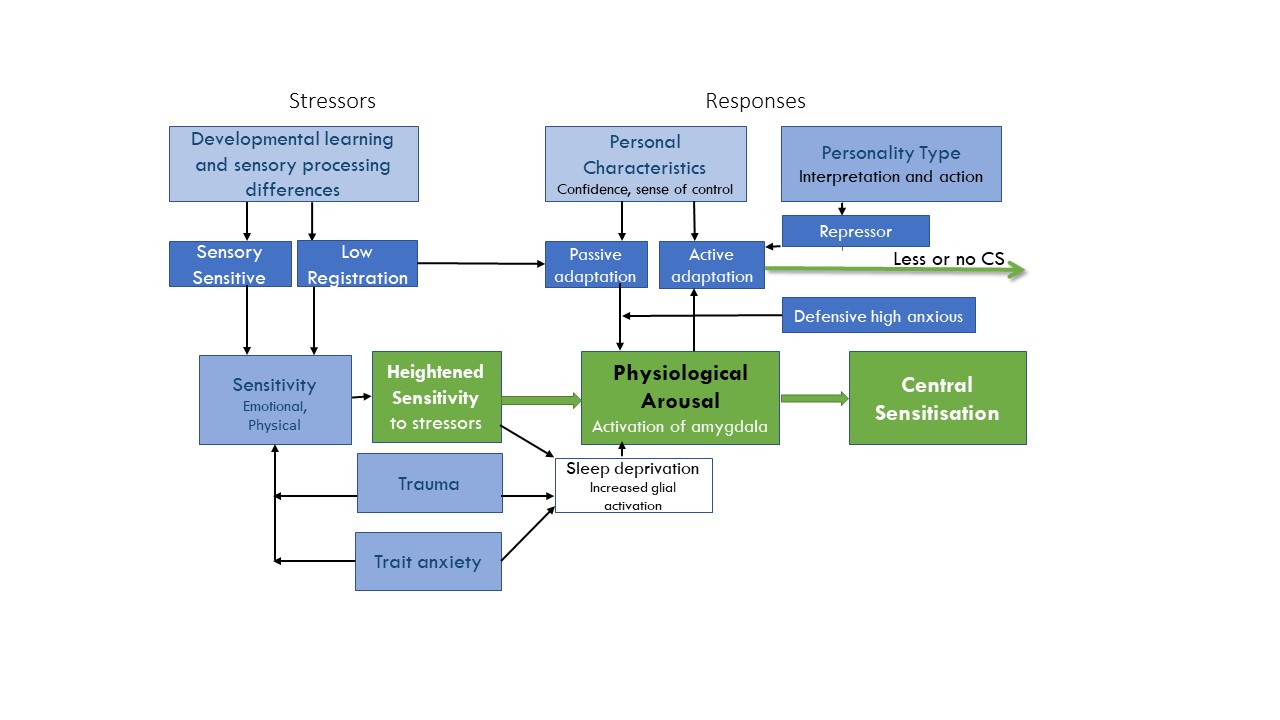
Figure 1: Diagram to summarise our proposal that pre-morbid contexts and characteristics of trait anxiety and sensory processing extremes may lead to heightened sensitivity and physiological arousal to stressors, and a personality type-dependent response. A response of attention towards, and interpretation for, threat-related stimuli may lead to CS symptoms in people with NSCLBP.
Implications
In the clinic, when an individual can identify their personality traits and sensory processing tendencies, this can enhance their understanding of themselves in relation to CS pain. Understanding that they may need to actively respond to physiological arousal from stressors by reducing excessive sensory stimulation, or indeed by increasing particular stimulation (Low Registration), to function more healthily may empower individuals to feel more in control. For the therapist, understanding the defensive high anxious and repressor individuals may enable better tailoring of pain neuroscience education. Our studies have paved the way for further investigation into predicting who develops CS pain and who recovers, after a back pain or injury.
Dr. Jacqui Clark
2020Pain in Motion
References and further reading:
Franklin, Z., Smith, N., & Fowler, N. (2014). Defensive high-anxious individuals with chronic back pain demonstrate different treatment choices and patient persistence. Personality and Individual Differences, 64(0), 84-88. doi:http://dx.doi.org/10.1016/j.paid.2014.02.020
Nijs, J., Apeldoorn, A., Hallegraeff, H., Clark, J., Smeets, R., Malfliet, A., . . . Ickmans, K. (2015). Low back pain: guidelines for the clinical classification of predominant neuropathic, nociceptive, or central sensitization pain. Pain Physician, 18(3), E333-346.
Nijs, J., Loggia, M. L., Polli, A., Moens, M., Huysmans, E., Goudman, L., . . . Clauw, D. (2017). Sleep disturbances and severe stress as glial activators: key targets for treating central sensitization in chronic pain patients? Expert Opinion on Therapeutic Targets, 21(8), 817-826. doi:10.1080/14728222.2017.1353603
Smart, K. M., Blake, C., Staines, A., Thacker, M., & Doody, C. (2012). Mechanisms-based classifications of musculoskeletal pain: Part 1 of 3: Symptoms and signs of central sensitisation in patients with low back (±leg) pain. Manual Therapy, 17(4), 336-344. doi:10.1016/j.math.2012.03.013