“Pain is in the brain” is no longer a novel statement in the field of pain research, but can be regarded as one of the main pillars of most recent thinking models about pain in the last decades. This statement highlights that the focus in pain -and especially chronic pain- research has been shifted from a biomedical peripheral tissue injury perspective towards the study of the structure and function of the brain, and by extension the whole central nervous system. Studying the brain is merited by and based upon the fact that the central nervous system (CNS) plays a crucial role in the transfer and processing of (noxious) signals, the subsequent interpretation of ‘pain’ itself and often undergoes neuroplastic changes when in pain (Apkarian et al. 2005; Farmer et al. 2012; Flor et al. 1997; Philips et al. 2011; Tracey et al. 2009).
Despite the fact that this is nothing new, as studying the CNS already forms an integral part of pain research since decades, still only the tip of the iceberg has been unraveled regarding the ‘low back pain brain’. Chronic low back pain (CLBP) is still the number 1 disabling chronic pain syndrome of our modern society, with prevalence and incidence rates increasing despite the vast amount of research being done in this field. (Dagenais et al. 2008; Henchoz et al. 2013; Vos et al. 2016)
The ‘low back pain brain’ can be studied with regards to its structural and functional properties. (Functional) magnetic resonance imaging (MRI/fMRI) is a commonly used imaging technique that studies both of these aspects. Brain alterations in LBP found with these techniques have already been summarized in two systematic reviews. (Kregel et al. 2015; Ng et al. 2018) Without going too much into detail the main findings of these reviews regarding chronic low back (CLBP) were as follows: Moderate evidence for regional and global changes in brain structure in CLBP were described. These changes indicated a likely decrease of gray matter brain volume in areas responsible for planning and executive functions, sensory-emotional processes and memory. Concerning white matter, evidence was more ambiguous as both increases and decreases in white matter volume were found, often also depending on the studied areas (Kregel et al. 2015;Ng et al. 2018). Functional alterations like changed functional connectivity in the default mode network at rest (Kregel et al. 2015; Ng et al. 2018), higher activity in pain-related brain areas and lower activity in analgesic brain areas were found in response to noxious stimuli. Furthermore, several specific tasks were also related to altered brain function (Kregel et al. 2015) (for a detailed description see reviews: Ng et al. 2018; Kregel et al. 2018).
Due to its high spatial resolution (f)MRI has a lot of merit for studying the brain, however its temporal resolution is rather low and (f)MRI can only be used in laboratory settings with subjects lying down in the device. Furthermore, the financial costs for this type of research are very high. In order to measure brain functional processes that often only occur for a couple of milliseconds, imaging techniques with a higher temporal resolution are needed as well. And this is where electroencephalography (EEG) comes into the picture. EEG is a technique that measures bio-electrical potentials that are a byproduct of underlying brain activity. This technique is optimally suited for the study of function of the LBP brain, due to its very high temporal resolution that makes it possible to measure instantaneous changes in brain activity (Hämäläinen et al. 1993). Furthermore, it is cheaper and easier-to-use than (f)MRI, with recent mobile or even wireless applications allowing for measurement during functional tasks in different bodily positions outside laboratory settings and even during whole body movement tasks.
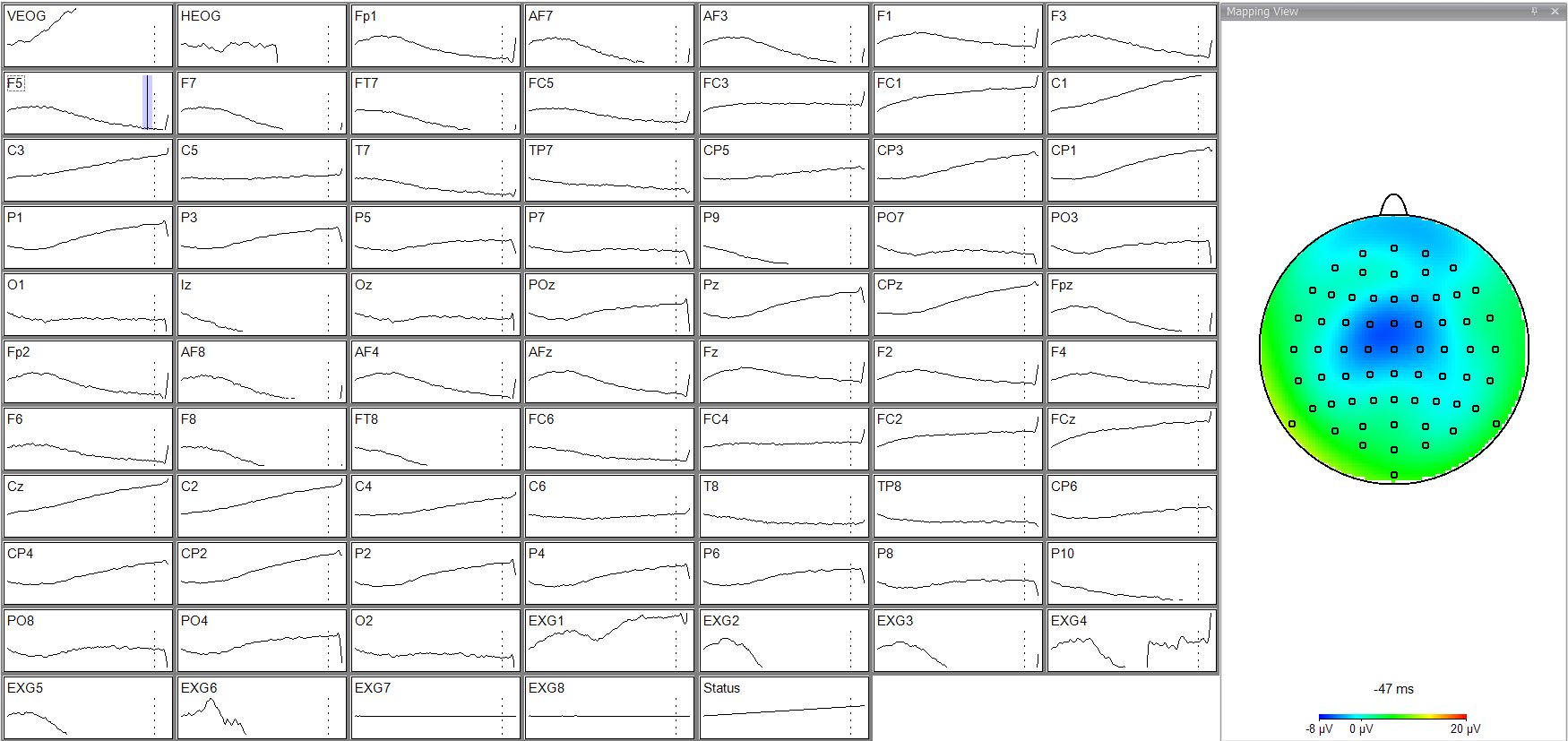
The functional division of the brain consists of sensory processing (Becker et al. 1993; Bromm et al. 1984; Bromm et al. 2001; Bushnell et al. 1999; Chapman et al. 1984; Chen et al. 1979; Erwin et al. 1986; Miltner et al. 1988; Price et al. 1988; Tarkka et al. 1993; Treede et al. 1998), cognitive-emotional processing (Donchin et al. 1988; Hillyard et al. 1973; Johnson et al. 1988; Lee et al. 2014), motor planning and execution (Bolton et al. 2015; Brunia et al. 2003; Jankelowitz et al. 2002; Marlin et al. 2014; Mierau et al. 2015; Mochizuki et al. 2009; Mochizuki et al. 2008; Quant et al. 2004; Shibasaki et al. 2006), speech (Ganushchak et al. 2011), and executive functions, reasoning and planning of complex behavior (Cui et al. 2013; Ferdinand et al. 2013; Hillyard et al. 1973; Schuermann et al. 2011), all of which have been examined with EEG in healthy populations. However, a clear synthesis of studies examining functional brain alterations in LBP populations with EEG does not yet exist, despite the fact that this might be of value for further understanding the chronification process in LBP. Furthermore, such an overview could guide further research by pointing out lacunas or forgotten territory in current research that still need to be discovered.
Therefore, our research group (SPINE Research Unit Ghent, Ghent University) is currently performing a systematic review that aims at synthesizing what alterations in function in the ‘low back pain brain’ compared to a ‘healthy brain’ (if this even exists) have already been discovered with EEG, as this might help clarify the chronification process in (C)LBP. Furthermore, recommendations for future research with EEG that might help clarify the below-surface vast chunk of iceberg in (C)LBP chronicity that is yet to be discovered will be made as well. As this study is not yet published, we hope to be able to present full results of this review on the upcoming Pain Science in Motion conference in Savona (May 2019).
With this blogpost we wished to highlight the important role of brain imaging, and more specifically EEG, to further examine (C)LBP as this might help elucidate the chronification process in these patients and can amplify the knowledge about specific functional processes that might accompany (C)LBP.
Poll: Do you think EEG is a useful technique for further unravelling low back pain brain function?
Vote: https://linkto.run/p/C5S8J79Q
Results: https://linkto.run/r/C5S8J79Q

Stijn Schouppe
Stijn Schouppe obtained his Master’s degree in Physiotherapy and Rehabilitation Sciences in 2015 from the University of Ghent, Belgium. For his Master thesis, he examined intradiscal pressure in concordance with kinematic measures in an in vitro study performed on human cadavers. In 2016 he obtained the postgraduate degree of ‘Manual Therapist’ at Ghent University. He is currently active as a PhD student in the Spine Research Unit of Ghent University. His main research interests are related to sensorimotor control, movement performance and the connection of these factors with psychosocial and cognitive-affective dimensions in the different low back pain populations. In 2016 Stijn became a member of the international Pain in Motion research group.
2018 Pain in Motion
References and further reading:
Apkarian AV, Bushnell MC, Treede RD, Zubieta JK. Human brain mechanisms of
pain perception and regulation in health and disease. European journal of pain
2005;9(4):463-484.
https://www.ncbi.nlm.nih.gov/pubmed/15979027
Becker DE, Yingling CD, Fein G. Identification of pain, intensity and P300
components in the pain evoked potential. Electroencephalography and clinical
neurophysiology 1993;88(4):290-301.
Bolton DA. The role of the cerebral cortex in postural responses to externally
induced perturbations. Neuroscience and biobehavioral reviews 2015;57:142
155.
https://www.ncbi.nlm.nih.gov/pubmed/26321589
Bromm B. Pain-related components in the cerebral potential, experimental and
multivariate statistical approaches. In: B Bromm, editor. Pain measurement in
man. Amsterdam: Elsevier, 1984. pp. 257-290.
Bromm B. Brain images of pain. News in physiological sciences : an international
journal of physiology produced jointly by the International Union of
Physiological Sciences and the American Physiological Society 2001;16:244-249.
https://www.ncbi.nlm.nih.gov/pubmed/11572930
Brunia CHM. CNV and SPN: Indices of Anticipatory Behavior. In: M Jahanshahi,
M Hallett, editors. The Bereitschaftspotential: Movement-Related Cortical
Potentials. Boston, MA: Springer US, 2003. pp. 207-227.
https://link.springer.com/chapter/10.1007/978-1-4615-0189-3_13
Bushnell MC, Duncan GH, Hofbauer RK, Ha B, Chen JI, Carrier B. Pain
perception: is there a role for primary somatosensory cortex? Proceedings of
the National Academy of Sciences of the United States of America
1999;96(14):7705-7709.
https://www.ncbi.nlm.nih.gov/pubmed/10393884
Chapman CR, Jacobson RC. Assessment of analgesic states:Can evoked
potentials play a role. In: B Bromm, editor. Pain measurement in man.
Amsterdam: Elsevier, 1984. pp. 233-256.
Chen AC, Chapman CR, Harkins SW. Brain evoked potentials are functional
correlates of induced pain in man. Pain 1979;6(3):365-374.
https://www.ncbi.nlm.nih.gov/pubmed/460937
Cui JF, Chen YH, Wang Y, Shum DH, Chan RC. Neural correlates of uncertain
decision making: ERP evidence from the Iowa Gambling Task. Front Hum
Neurosci 2013;7:776.
https://www.ncbi.nlm.nih.gov/pubmed/24298248
Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of
illness studies in the United States and internationally. The spine journal :
official journal of the North American Spine Society 2008;8(1):8-20.
https://www.ncbi.nlm.nih.gov/pubmed/18164449
Donchin E, Coles M. Is the P300 component a manifestation of context
updating? Behavioral and Brain Sciences 1988;11(3):357-427.
Erwin R, Buchwald JS. Midlatency auditory evoked responses: differential
effects of sleep in the human. Electroencephalography and clinical
neurophysiology 1986;65(5):383-392.
https://www.ncbi.nlm.nih.gov/pubmed/2427329
Farmer MA, Baliki MN, Apkarian AV. A dynamic network perspective of chronic
pain. Neuroscience letters 2012;520(2):197-203.
https://www.ncbi.nlm.nih.gov/pubmed/22579823
Ferdinand NK, Kray J. Age-related changes in processing positive and negative
feedback: is there a positivity effect for older adults? Biological psychology
2013;94(2):235-241.
https://www.ncbi.nlm.nih.gov/pubmed/23886960
Flor H, Braun C, Elbert T, Birbaumer N. Extensive reorganization of primary
somatosensory cortex in chronic back pain patients. Neuroscience letters
1997;224(1):5-8.
https://www.ncbi.nlm.nih.gov/pubmed/9132689
Ganushchak LY, Christoffels IK, Schiller NO. The Use of Electroencephalography
in Language Production Research: A Review. Frontiers in Psychology
2011;2:208.
https://www.ncbi.nlm.nih.gov/pubmed/21909333
Hämäläinen M, Hari R, Ilmoniemi R, Knuutila J, V. Lounasmaa O.
Magnetoencephalography: Theory, instrumentation, and applications to
noninvasive studies of the working human brain, Vol. 65, 1993.
Henchoz Y, Tetreau C, Abboud J, Piche M, Descarreaux M. Effects of noxious
stimulation and pain expectations on neuromuscular control of the spine in
patients with chronic low back pain. The spine journal : official journal of the
North American Spine Society 2013;13(10):1263-1272.
https://www.ncbi.nlm.nih.gov/pubmed/24090825
Hillyard SA, Hink RF, Schwent VL, Picton TW. Electrical signs of selective
attention in the human brain. Science (New York, NY) 1973;182(4108):177-180.
https://www.ncbi.nlm.nih.gov/pubmed/4730062
Jankelowitz SK, Colebatch JG. Movement-related potentials associated with
self-paced, cued and imagined arm movements. Experimental brain research
2002;147(1):98-107.
https://www.ncbi.nlm.nih.gov/pubmed/12373374
Johnson R. The amplitude of the P300 component of the event-related
potential: Review and synthesis. Advances in Psychophysiology 1988;3.
Kregel J, Meeus M, Malfliet A, Dolphens M, Danneels L, Nijs J, Cagnie B.
Structural and functional brain abnormalities in chronic low back pain: A
systematic review. Seminars in arthritis and rheumatism 2015;45(2):229-237.
https://www.ncbi.nlm.nih.gov/pubmed/26092329
Lee YY, Hsieh S. Classifying different emotional states by means of EEG-based
functional connectivity patterns. PloS one 2014;9(4):e95415.
https://www.ncbi.nlm.nih.gov/pubmed/24743695
Marlin A, Mochizuki G, Staines WR, McIlroy WE. Localizing evoked cortical
activity associated with balance reactions: does the anterior cingulate play a
role? Journal of neurophysiology 2014;111(12):2634-2643.
https://www.ncbi.nlm.nih.gov/pubmed/24647435
Mierau A, Hulsdunker T, Struder HK. Changes in cortical activity associated with
adaptive behavior during repeated balance perturbation of unpredictable
timing. Front Behav Neurosci 2015;9:272.
https://www.ncbi.nlm.nih.gov/pubmed/26528154
Miltner W, Larbig W, Braun C. Biofeedback of somatosensory event-related
potentials: can individual pain sensations be modified by biofeedback-induced
self-control of event-related potentials? Pain 1988;35(2):205-213.
https://www.ncbi.nlm.nih.gov/pubmed/3237434
Mochizuki G, Sibley KM, Cheung HJ, Camilleri JM, McIlroy WE. Generalizability
of perturbation-evoked cortical potentials: Independence from sensory, motor
and overall postural state. Neuroscience letters 2009;451(1):40-44.
https://www.ncbi.nlm.nih.gov/pubmed/19110034
Mochizuki G, Sibley KM, Esposito JG, Camilleri JM, McIlroy WE. Cortical
responses associated with the preparation and reaction to full-body
perturbations to upright stability. Clinical neurophysiology : official journal of
the International Federation of Clinical Neurophysiology 2008;119(7):1626
1637.
https://www.ncbi.nlm.nih.gov/pubmed/18479966
Ng SK, Urquhart DM, Fitzgerald PB, Cicuttini FM, Hussain SM, Fitzgibbon BM.
The Relationship Between Structural and Functional Brain Changes and Altered
Emotion and Cognition in Chronic Low Back Pain Brain Changes: A Systematic
Review of MRI and fMRI Studies. The Clinical journal of pain 2018;34(3):237
261.
https://www.ncbi.nlm.nih.gov/pubmed/28719509
Phillips K, Clauw DJ. Central pain mechanisms in chronic pain states--maybe it is
all in their head. Best practice & research Clinical rheumatology 2011;25(2):141
154.
https://www.ncbi.nlm.nih.gov/pubmed/22094191/
Price DD. Psychological and neural mechanisms of pain. New York: Raven Press,
1988. pp. 1-18.
https://onlinelibrary.wiley.com/doi/abs/10.1002/syn.890040111
Quant S, Adkin AL, Staines WR, McIlroy WE. Cortical activation following a
balance disturbance. Experimental brain research 2004;155(3):393-400.
https://www.ncbi.nlm.nih.gov/pubmed/14968271
Schuermann B, Kathmann N, Stiglmayr C, Renneberg B, Endrass T. Impaired
decision making and feedback evaluation in borderline personality disorder.
Psychological medicine 2011;41(9):1917-1927.
https://www.ncbi.nlm.nih.gov/pubmed/22094191
Shibasaki H, Hallett M. What is the Bereitschaftspotential? Clinical
neurophysiology : official journal of the International Federation of Clinical
Neurophysiology 2006;117(11):2341-2356.
https://www.ncbi.nlm.nih.gov/pubmed/16876476
Tarkka IM, Treede RD. Equivalent electrical source analysis of pain-related
somatosensory evoked potentials elicited by a CO2 laser. Journal of clinical
neurophysiology : official publication of the American Electroencephalographic
Society 1993;10(4):513-519.
https://www.ncbi.nlm.nih.gov/pubmed/8308146
Tracey I, Bushnell MC. How neuroimaging studies have challenged us to rethink:
is chronic pain a disease? The journal of pain : official journal of the American
Pain Society 2009;10(11):1113-1120.
https://www.ncbi.nlm.nih.gov/pubmed/19878862
Treede RD, Meyer RA, Campbell JN. Myelinated mechanically insensitive
afferents from monkey hairy skin: heat-response properties. Journal of
neurophysiology 1998;80(3):1082-1093.
https://www.ncbi.nlm.nih.gov/pubmed/9744923
Vos T, Allen C, Arora M, et al. Global, regional, and national incidence, prevalence,
and years lived with disability for 310 diseases and injuries, 1990–2015: a
systematic analysis for the Global Burden of Disease Study 2015. The Lancet
2016;388(10053):1545-1602.