A universally accepted term for the phenomenon ‘central sensitization’ in humans is not available yet and a proof of this fact is that its use in scientific literature is still under debate (Kosek et al. 2016). Despite growing awareness in the last years of the contribution of altered central pain processing in a subgroup of patients with knee osteoarthritis pain, routine evaluation of central sensitization is yet to be incorporated into clinical practice.
In part this might be due to the historical laboratory-based focus of central sensitization research, where the equipment and protocols used to identify features of central sensitization are relatively heterogeneous, sophisticated, and often not clinically pragmatic.
With this background in mind, nine clinicians and researchers from seven different countries have recently summarized, in a non-systematic manner and by using the current understanding of central sensitization within the context of knee osteoarthritis pain, a set of clinical descriptors for the recognition of possible dominant central sensitization in patients with knee osteoarthritis (Lluch et al. 2017). At this moment these descriptors should not be considered unique diagnostic signs indicating central sensitization. Central sensitization is not a diagnosis nor an illness and therefore it is not suitable to develop diagnostic criteria. These descriptors should be considered as potential candidates for indicating central sensitization in people with knee osteoarthritis that should be tested in future research.
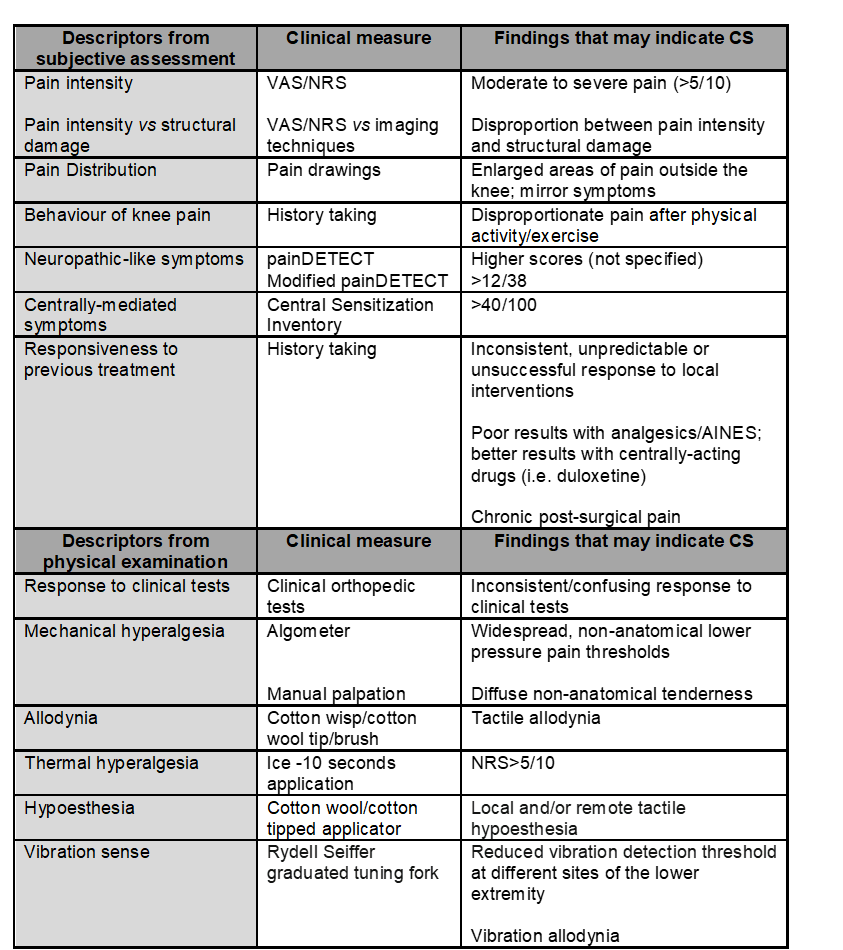
The clinical descriptors do not aim to replace the laboratory-based investigation of central sensitization, but do aim to bridge the gap between research findings and clinical practice by translating the laboratory-based studies of central sensitization into a more clinically-relevant perspective. For a better comprehension, these descriptors are structured into two categories: descriptors derived from the subjective assessment (subjective descriptors) and descriptors extracted from the physical examination (objective descriptors). In the table, you can find a checklist with all clinical descriptors aiding clinicians to recognize central sensitization in patients with knee osteoarthritis.
The validity of these clinical descriptors as classification tool is still unsubstantiated, so their psychometric properties should be the subject of future research to allow them to be confidently adopted in clinical practice. Meanwhile, they may hopefully be integrated into clinicians’ clinical reasoning in order to facilitate clinicians’ acknowledgment and recognition of central sensitization in people with knee osteoarthritis.
Enrique Lluch
2017 Pain in Motion
References and further reading:
Kosek E, Cohen M, Baron R, et al. Do we need a third mechanistic descriptor for chronic pain states? Pain. 2016;157:1382-6.
https://www.ncbi.nlm.nih.gov/pubmed/26835783
Lluch E, Nijs J, Courtney CA, Rebbeck T, Wylde V, Baert I, Wideman TH, Howells N, Skou ST. Clinical descriptors for the recognition of central sensitization pain in patients with knee osteoarthritis. Disabil Rehabil. 2017:1-10.