COVID-19, a highly infectious disease that was first reported in Wuhan in China in December 2019, has definitely changed our behaviour. COVID-19 is caused by the SARS-CoV-2 virus. The World Health Organisation has declared COVID-19 as a pandemic on March 11th, 2020 due to the rapid increase in number of confirmed cases (Wang et al. 2020). The virus has spread quickly outside China to Europe, United States, ... and has been detected in 213 countries and territories up till now. This infectious disease is challenging epidemiologists, methodologists and statisticians who hold the responsibility to inform the government about a broad gamma of issues and guidelines, related to this outbreak. The impact of guidelines such as social distancing and isolation is not to be underestimated. Data recorded just two weeks into the China outbreak of COVID-19 revealed that more than 50% of the respondents rated the psychological impact of this outbreak as moderate or severe (Wang et al. 2020).
Karos et al. (2020) elaborated on the different social threats of COVID-19 for people with chronic pain (Karos et al. 2020). One of the most straightforward effects of the pandemic was the introduction of physical distancing measures and restrictions to travel. Social isolation is associated with loneliness, higher levels of depression or anxiety, poorer sleep and pain. Chronic pain itself places individuals at an increased risk of social isolation with smaller social network sizes and potentially reduced social role functioning. Due to the obligatory physical distance rules and reduced participation due to COVID-10, a steep rise in prevalence of loneliness is expected. Especially in persons living with chronic pain, who may have started with a smaller social network, a higher proportion of patients with loneliness and social disconnection is expected. As such, it is obvious that chronic pain patients are even at a higher risk for developing depression during this pandemic since social isolation itself is a risk factor for the development of depressive symptoms (Herbolsheimer et al. 2018). Karos et al. also acknowledged that being isolated from the community forces people to life in closer proximity to household members. Closer proximity to others might improve social bonds and thereby form a buffer against pain. However, the opposite is also possible whereby an increase in solicitous behaviours can unintentionally contribute to the chronicity of pain. A third problem is the reduced access to high-quality healthcare. In general, the greatest part of daily chronic pain services activity is considered as non-urgent, whereby the majority of activities related to chronic pain services (e.g. consultations) were interrupted or reduced (Piraccini et al. 2020). Lastly, an exacerbation of social injustice and social inequalities might pop up. On the one hand, physical distancing policies might be the driver to increase social isolation and potentially worsen perceived injustices. Disrupting social networks that are sources of justice and support, on the other hand, may stimulate perceptions of invalidation among those with pain. Figure 1 is providing an overview of the different social threats according to Karos et al. (2020).
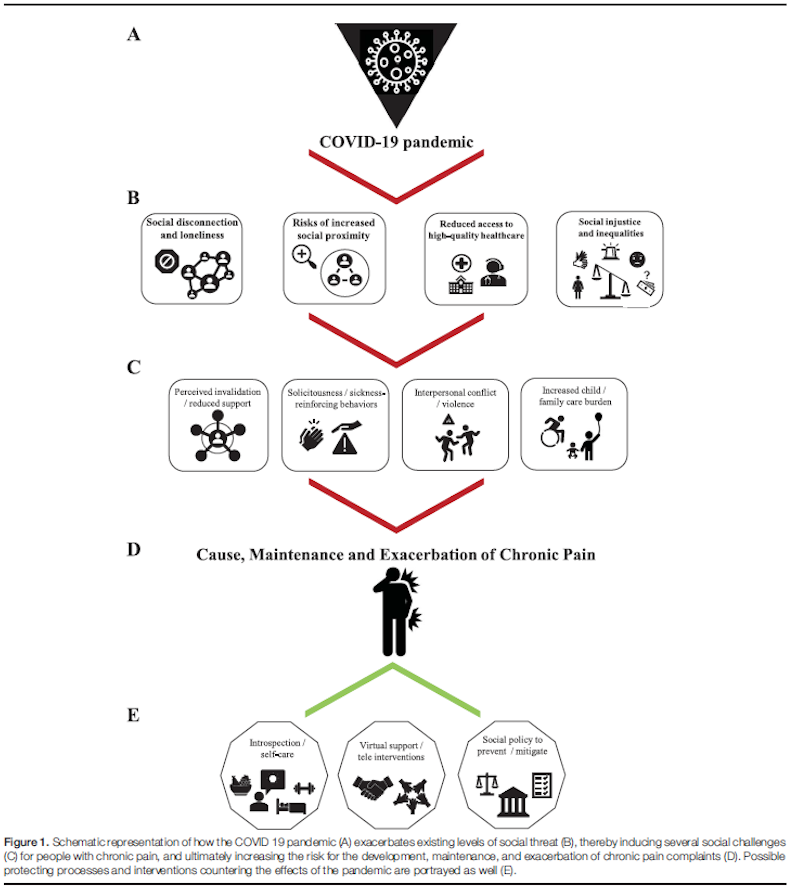
Figure 1: different social threats of COVID-19 in chronic pain patients (according to Karos et al. (2020)).
It thus becomes clear that the wide range of social threats that COVID-19 brings to chronic pain patients, requires a focused and targeted approach. One of the solutions that have been implemented in clinical practice was the efficient use of technology. Social media platforms can help disseminate key information about the pandemic and provide virtual support to enhance social connections. As such, online peer-support may help to reduce the feeling of loneliness and increase social contacts. Additionally, telemedicine has rapidly expanded and been applied to the field of chronic pain to perform consultations remotely. Several benefits have been reported like psychosocial and motivational factors, convenience, improved access and comprehensive evaluations can be performed remotely (Emerick et al. 2020). Despite some disadvantages of the current technology (for example limited ability to perform a physical examination or financial considerations), COVID-19 might have changed the landscape of chronic pain management. A couple of innovations like remote monitoring of vital signs, consolidations of electronic medical record systems and a comprehensive evaluation of self-reporting over the Internet might endure after this pandemic and could positively influence pain management in the future (Emerick et al. 2020).
Lisa Goudman
2020 Pain in Motion
References and further reading:
Emerick, T., B. Alter, S. Jarquin, S. Brancolini, C. Bernstein, K. Luong, S. Morrisseyand and A. Wasan (2020). "Telemedicine for Chronic Pain in the COVID-19 Era and Beyond." Pain Med 21(9): 1743-1748. https://pubmed.ncbi.nlm.nih.gov/32914858/
Herbolsheimer, F., N. Ungar and R. Peter (2018). "Why Is Social Isolation Among Older Adults Associated with Depressive Symptoms? The Mediating Role of Out-of-Home Physical Activity." Int J Behav Med 25(6): 649-657. https://pubmed.ncbi.nlm.nih.gov/30350258/
Karos, K., J. L. McParland, S. Bunzli, H. Devan, A. Hirsh, F. P. Kapos, E. Keogh, D. Moore, L. M. Tracy and C. E. Ashton-James (2020). "The social threats of COVID-19 for people with chronic pain." Pain 161(10): 2229-2235. https://pubmed.ncbi.nlm.nih.gov/32694381/
Piraccini, E., H. Byrne and S. Taddei (2020). "Chronic pain management in COVID-19 era." J Clin Anesth 65: 109852. https://pubmed.ncbi.nlm.nih.gov/32361284/
Wang, C., R. Pan, X. Wan, Y. Tan, L. Xu, C. S. Ho and R. C. Ho (2020). "Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China." Int J Environ Res Public Health 17(5). https://pubmed.ncbi.nlm.nih.gov/32155789/
Wang, J. and Z. Wang (2020). "Strengths, Weaknesses, Opportunities and Threats (SWOT) Analysis of China's Prevention and Control Strategy for the COVID-19 Epidemic." Int J Environ Res Public Health 17(7). https://pubmed.ncbi.nlm.nih.gov/32225019/