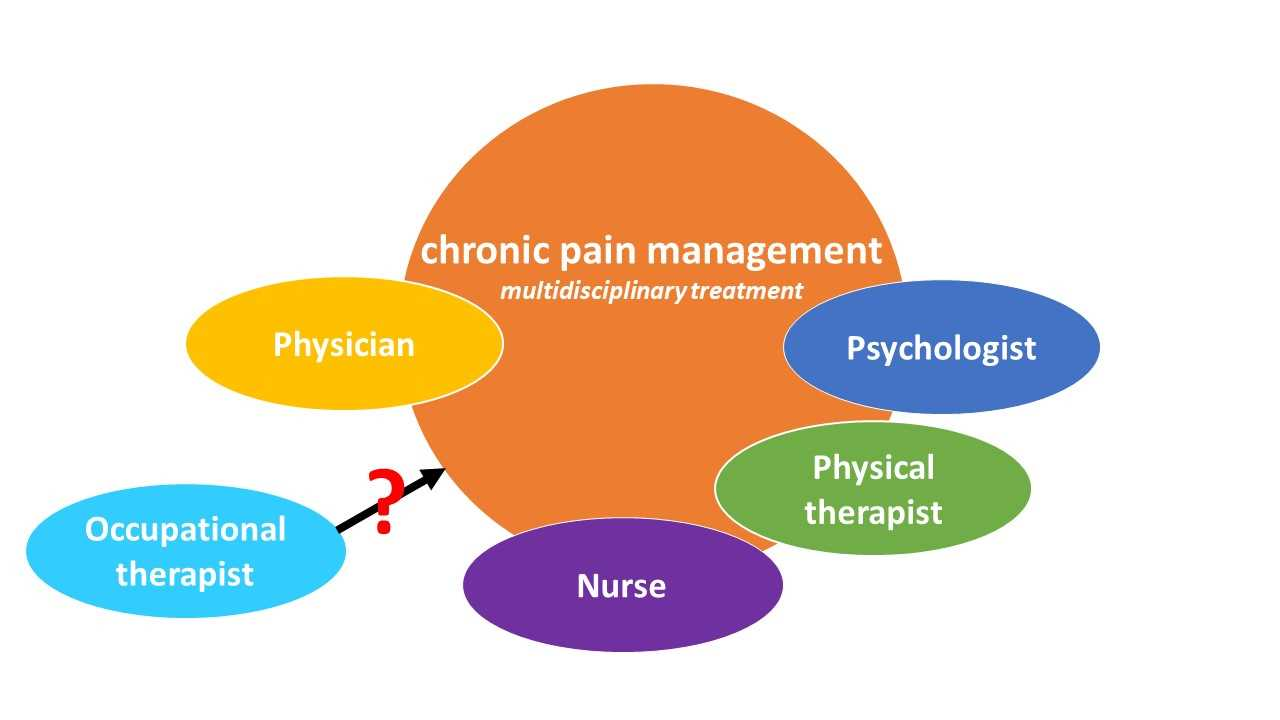
This is a question that all patients, the multidisciplinary rehabilitation team and more importantly all occupational therapists should ask.
Chronic pain is common in Europe and affects a high number of adults from an, what we ought to be, active age group. Prevalence of chronic pain was reported to increase from 18 to 40 years and to be highest in the 41-50 age group. Disease duration is also not something to overlook. Most respondents in the study of Breivik et al. reported to suffer from chronic pain from 2 to 15 years. Based on these numbers, we cannot be surprised that chronic pain has a large impact on the performance of daily life activities (Breivik et al. 2006; Hesselstrand et al. 2015). Most limitations, i.e. being unable to perform, were reported on work activities (32%), followed by driving (23%), lifting (23%) and exercising (23%). When asked which activities patients with chronic pain were less able to perform, highest limitations were found in ability to sleep (56%), exercise (50%), lift (49%), perform household activities (42%) and walk (40%) (Breivik et al. 2006).
Patients who are unable to take initiative and perform meaningful work or educational, household and/or social or leisure activities, and thus are unable to participate (Borell et al. 2006), can experience a loss of identity because they cannot fulfil their expected roles (Harris et al. 2003; van Huet et al. 2013). This can lead to the inability of occupational performance (Breivik et al. 2006; Skjutar et al. 2010) and loss of quality of life (American Academy of Family Physicians 2000; Robinson et al. 2011a;). On the other hand, chronic pain also has a high, negative impact on a country’s economy due to work force and health care costs (National Research Council and Institute of Medicine 2001).
Because the inability to participate has a negative impact on a person’s health and because occupational therapy (OT) acknowledges and uses the power of occupation to increase quality of life (Peloquin 1991), occupational therapists should have an important role in and contribute to chronic pain management.
Robinson et al. and Jakobs et al. reviewed the state of the art concerning chronic pain management and the (possible) role of the occupational therapist.
Chronic pain management is found to be most effective when performed by a multidisciplinary rehabilitation team (Busch et al. 2011; Gatchel & Okifuji 2006). However, when reviewing scientific literature, it is unclear which roles or interventions are best performed by occupational therapists in relation to their expertise (Robinson et al. 2011b; Jakobs et al. 2014).
Skjutar et al. investigated occupational therapists’ point of view on the need for OT in patients with chronic pain. Limitations in occupational performance were identified as the overall need, with pain behavior, lack of knowledge, occupational imbalance, emotional stress and physical or environmental strain as subthemes. When comparing results to patients’ perspectives on the need for OT, more psychologically-based indicators, such as low self-efficacy, problems adapting to a new life, problems meeting external expectations, increasing pain and longing to be at work despite sick leave were not identified by the professionals (Müllersdorf et al. 2002; Skjutar et al. 2010). Improving occupational performance with more attention to psychological factors in all important areas of life should be OTs’ focus (Skjutar et al. 2010).
Evidence identifies cognitive behavioral therapy (CBT) as the most appropriate intervention (Gatchel & Okifuji 2006), but occupational therapists should be careful to not just copy this intervention, as it is psychologically-based and does not sufficiently fit in with their professional domain, as argued by Robinson and colleagues. Graded activity and graded exposure are two other multidisciplinary treatment methods which are found effective for chronic pain, but are not yet fully adopted by occupational therapists in clinical practice. Scientific research advocates that occupational therapists could play an important role in these three interventions, but it needs to be further investigated how they fit with their expertise and professional domain (Robinson et al., 2011b; Jakobs et al. 2014).
Robinson et al. mentioned three important ‘red flags’ concerning OT for chronic pain:
With their review, they point at the necessity for further research focusing on the outcomes of occupation-based interventions. This in order to prevent that other professionals develop expertise in the use of activity and consequently replace the role of the occupational therapists. Next, to assure that applied interventions fit within the professional domain of the occupational therapist and match the needs of patients with chronic pain. Until then, they stress that occupational therapists should make more use of appropriate and relevant scientific evidence that supports their occupational therapy practice.
Up to now, there is still too little evidence available for OT in patients with chronic pain. We should not lose sight of this professional group and start investigating their role in chronic pain management, as they could have an important impact on the occupational performance and quality of life of patients with chronic pain.
Kuni Vergauwen
2018 Pain in Motion
References and further reading:
Breivik H, Collett B, Ventafridda V, Cohen R, & Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life and treatment. Eur J Pain 2006;10(4):287-333
https://www.ncbi.nlm.nih.gov/pubmed/16095934
Hesselstrand M, Samuelsson K, Liedberg G. Occupational therapy interventions in chronic pain: a systematic review. Occup Ther Int 2015;22(4):183-194.
https://www.ncbi.nlm.nih.gov/pubmed/26076994
Borell L, Asaba E, Rosenberg L, Schult M, Townsend E. Exploring experiences of ‘‘participation’’ among individuals living with chronic pain. Scand J Occup Ther 2006;13(2):76-85.
https://www.ncbi.nlm.nih.gov/pubmed/16856464
Harris S, Morley S, Barton S. Role loss and emotional adjustment in chronic pain. Pain 2003;105(1-2):363-370.
https://www.ncbi.nlm.nih.gov/pubmed/14499455
Van Huet H, Innes E, Stancliffe R. Occupational therapists perspectives of factors influencing chronic pain management. Aust Occup Ther J 2013;60(1),56-65.
https://www.ncbi.nlm.nih.gov/pubmed/23414190
Skjutar A, Schult M, Christensson K, Müllersdorf M. Indicators of need for occupational therapy in patients with chronic pain: occupational therapists’ focus groups. Occup Ther Int 2010;17(2),93-103.
https://www.ncbi.nlm.nih.gov/pubmed/19653210
American Academy of Family Physicians. (2000). Treatment of nonmalignant chronic pain. Retrieved January 13, 2018, from http://www.aafp.org/afp/20000301/1331.html
Robinson K, Kennedy N, Harmon D. Is Occupational Therapy adequately meeting the needs of people with chronic pain? Am J Occup Ther 2011a;65(1),106-113.
https://www.ncbi.nlm.nih.gov/pubmed/21309378
National Research Council and Institute of Medicine. (2001). Musculoskeletal disorders and the workplace: Low back pain and upper extremities. Washington, DC: National Academies Press.
https://www.ncbi.nlm.nih.gov/books/NBK222440/
Fisher GS, Emerson L, Firpo C, Ptak J, Wonn J, Bartolacci G. Chronic pain and occupation: an exploration of the lived experience. Am J Occup Ther 2007;61(3),290-302.
https://www.ncbi.nlm.nih.gov/pubmed/17569386
Peloquin SM. Occupational Therapy Service: Individual and Collective Understandings of the Founders, Part 1. Am J Occup Ther 1991;45(4):352-60.
https://www.ncbi.nlm.nih.gov/pubmed/2035607
Jakobs M, Meeus M, Huijnen I. Ergotherapie bij chronische pijn en chronisch vermoeidheidssyndroom. The state of the art. Wetenschappelijk tijdschrift voor ergotherapie 2014;7,3-4.
Busch H, Bodin L, Bergström G, Jensen IB. Patterns of sickness absence a decade after pain-related multidisciplinary rehabilitation. Pain 2011;152(8):1727-1733.
https://www.ncbi.nlm.nih.gov/pubmed/21507573
Gatchel RJ, Okifuji A. Evidence-based scientific data documenting the treatment and cost-effectiveness of comprehensive pain programs for chronic nonmalignant pain. J Pain 2006;7(11):779-93.
https://www.ncbi.nlm.nih.gov/pubmed/17074616
Robinson K, Kennedy N, Harmon D. Review of occupational therapy for people with chronic pain. Aust Occup Ther J 2011b;58(2),74-81.
https://www.ncbi.nlm.nih.gov/pubmed/21418229
Müllersdorf M. Needs and Problems Related to Occupational Therapy as Perceived by Adult Swedes with Long-Term Pain. Scand J Occup Ther 2002;9(2):79-90. http://www.tandfonline.com/doi/abs/10.1080/110381202320000061?journalCode=iocc20