INVITED BLOGPOST
For effective treatment of non-specific neck pain, physiotherapists should be able to rely on the evidence from scientific research. However, scientific research evidence is poorly integrated in physiotherapy. One possible cause for this poor integration is that RCTs do not reflect “the real world” of physiotherapy clinical reasoning.
A review of Maissan et al., 2018showed that 102 out of 122 RCTs included patients based on the presence pain. In addition, the second inclusion criterion was an age between 18 and 65 years. This means that only 20 RCTs also had additional inclusion criteria such as a limitation of Range of Motion (ROM) or a reduced muscle endurance. In 11 RCTs with specific diagnostic inclusion criteria, the treatment goal matched what was diagnosed and an appropriate outcome measures was used to monitor this goal. For example: first a decreased endurance of the neck musculature was diagnosed, then the intervention was endurance training with the goal to improve the endurance and finely the effect of the intervention was monitored with an endurance test. Therefore, these 11 RCTs had a clear linear line of clinical reasoning what makes it possible to understand this process and thus translatable to daily practice.
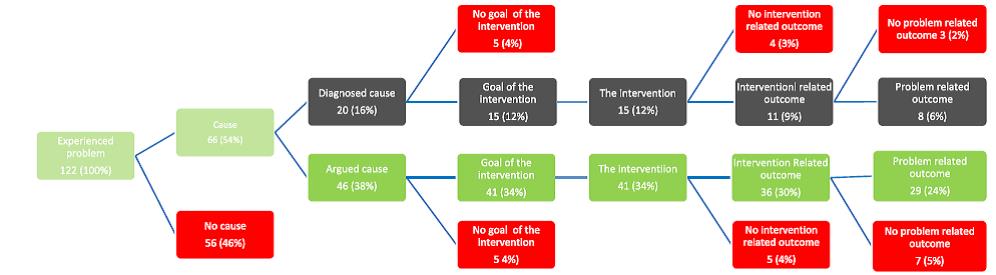
In studies with no diagnosed cause it remained unclear what the impairment, activity limitation or restriction in participation was. Thus, it is possible that in these studies the population did not have an impairment, activity limitation or restriction in participation at all. To illustrate; there were 5 studies aiming to improve neck Range of Motion (ROM), but the authors did not find any improvement in ROM. In these 5 studies the ROM at baseline was equal to norm values. Although some participants could have a ROM limitation, the possibility remains limited to achieve a good result if norm values are already measured at baseline. This could occur because a diagnosed ROM limitation was not used as an inclusion criterion. This example clearly emphasises the need to define and measure specific impairments, activity limitations or restriction in participation as inclusion criteria for participants.
In summary, a complete line of clinical reasoning appears to be of paramount importance for the examination of a specific intervention with its matching specific effect in order to understand working mechanisms of interventions.
The results of the review of Maissan et al., 2018were used as a starting point for a Web-based Delphi study (Maissan et al., 2018) in which 15 experts in treating people with non-specific neck pain participated. In this study we aimed to describe expert opinion on the indication for physiotherapy when a patient's only problem is pain without other signs or symptoms or positive diagnostic tests as happened in the earlier mentioned 102 RCTs. We also wanted to gain insight into their clinical reasoning. We hypothesized that if scientific research includes a clear clinical reasoning process, it should be easier to translate this reasoning into daily practice, especially by experts.
All experts considered physiotherapy treatment not indicated in patients with non-specific neck pain without any positive signs and/or symptoms or diagnostic tests other than pain alone. This would mean that in at least 102 RCTs no indication for physiotherapy had been established. Nonetheless, a physiotherapeutic intervention was investigated.
Despite the lenient boundary of consensus at >50%, only 6 out of 18 linear lines of clinical reasoning reached consensus. Possibly the poor translatability of RCTs contributed to this poor result. In our Delphi we found that in interventions to improve motor control or endurance consensus was reached. This can be explained when we look in more detail at a review of Maissan et al., 2018. This review showed that 4 RCTs to improve motor control or endurance were part of the 11 out of 122 RCTs with a complete clinical reasoning process. In other words, these RCTs included a diagnostic criterion to get a sub-group that matched with the intervention. Hence, it looks as if these research findings were easy to translate to clinical practice. Therefore, this seems to confirm the need to perform future research with a more clinically relevant focus.
Francois Maissan
Francois Maissan is a physical therapist and health scientist. He is also a PhD student at VU University Amsterdam, department Health science and Epidemiology.
2018 Pain in Motion
References and further reading:
The clinical reasoning process in randomized clinical trials with patients with non-specific neck pain is incomplete: A systematic review. Francois Maissan, Jan Pool, Edwin de Raaij, Jürgen Mollema, Raymond Ostelo, Harriet Wittink. Musculoskeletal Science and Practice, 2018, 35; 8–17
https://www.ncbi.nlm.nih.gov/pubmed/29413949
Clinical reasoning in unimodal interventions in patients with non-specific neck pain in daily physiotherapy practice, a Delphi study. Francois Maissan, Jan Pool, Eric Stutterheim, Harriet Wittink, Raymond Ostelo. Musculoskeletal Science and Practice, 2018, 37; 8–16