Unravelling low back pain remains a clinical challenge and the ideas about what can count as proper and necessary judgements are still a topic for debate. Recently, several groups have suggested that making distinctions between neuropathic pain and nociceptive pain in people with low back pain is important (Hush et al. 2013; Spahr et al. 2017).
According to the International Association for the Study of Pain (IASP), the definition of nociceptive pain is: 'Pain that arises from actual or threatened damage to non-neural tissue and is due to the activation of nociceptors'. The definition of neuropathic pain is: 'Pain caused by a lesion or disease of the somatosensory nervous system'. Referring to neuropathic pain, according to the IASP, a small group of low back pain patients will be classified as 'neuropathic'. Some patients describe signs and symptoms that are indicative for neuropathic components, but demonstrate no evidence for a lesion or disease of the somatosensory nervous system. It seems that low back pain patients with neuropathic pain do not always show the typical radicular symptoms.
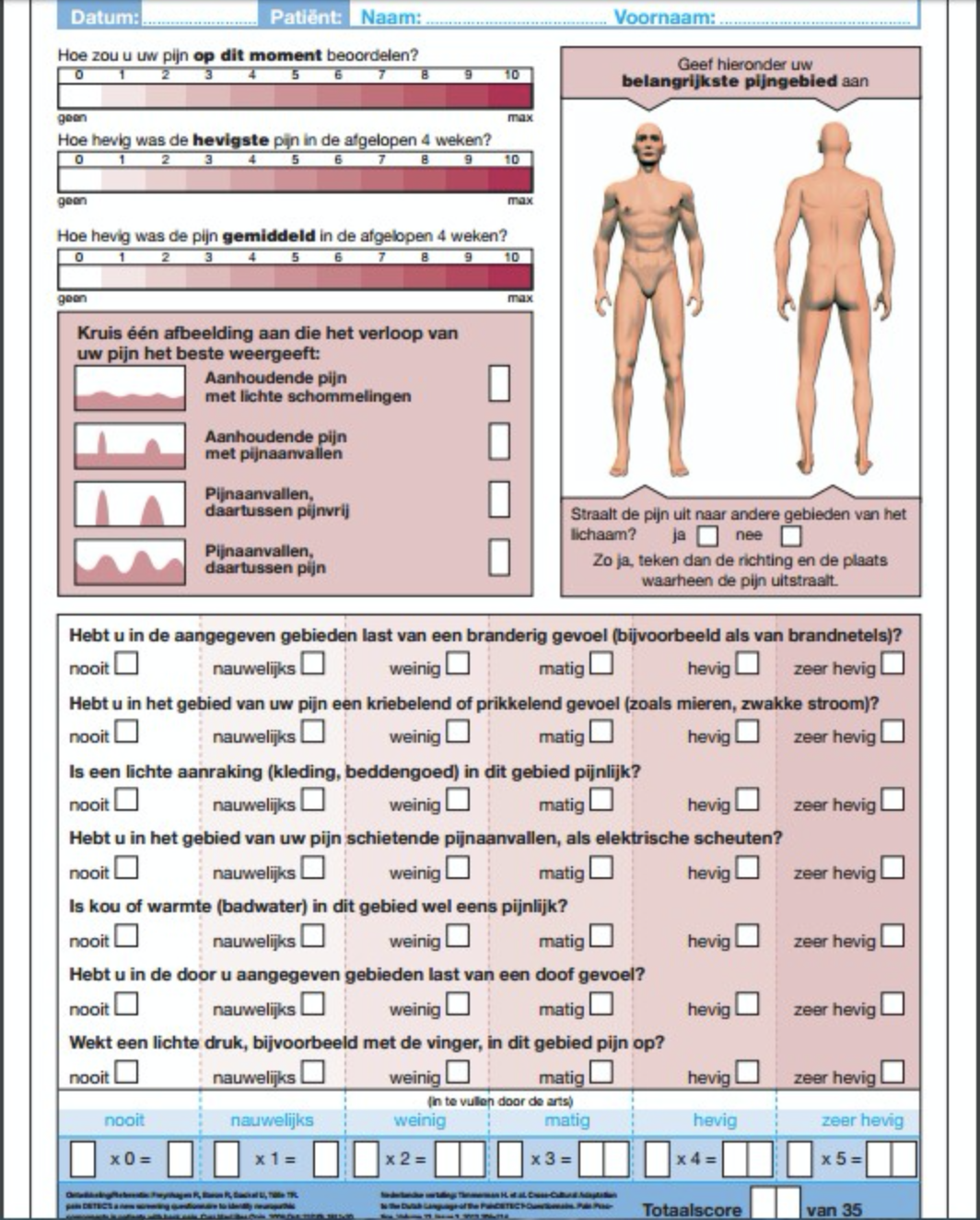
In a recent study, the proportion of patients with low back pain due to neuropathic mechanisms was determined using the painDETECT, an often used clinical tool for diagnosing neuropathic pain (Spahr et al. 2017). Spahr et al. included a sample of chronic low back pain patients and healthy controls and all participants filled in questionnaires (painDETECT, numeric rating scale, short form McGill Pain questionnaire, RAND Medical Outcomes 36-item Short Form Survey Instruments, Centre for Epidemiologic Studies Depression Scale Questionnaire, State Trait Anxiety Inventory and Revised Symptom Checklist 90 Questionnaire) and underwent sensory testing at the lower back (two-point discrimination and tactile threshold discrimination).
Participants who scored less than 19 points at the painDETECT questionnaire were classified as 'nociceptive mechanical pain' and participants who scored more than 19 points were classified as 'neuropathic components to their pain'.
The group with neuropathic components reported significantly higher day pain compared with the group with nociceptive pain. The group with neuropathic components showed significantly less physical and mental health related to quality of life than the group with nociceptive pain. The group with neuropathic components showed, compared with the group with nociceptive pain, more signs of depression and physical distress. Increased thresholds to tactile stimulation were found within the group with a neuropathic profile. No significant differences were reported between groups regarding two-point discrimination.
Spahr et al. assumed that participants with neuropathic components (established by the painDETECT) would have more pain, less quality of life, more psychological distress and different sensory testing profiles compared with the group with nociceptive pain. The results of their study confirm their hypotheses. The differences between groups were probably caused by other factors. For example, the pain intensity and psychological factors differed significantly between groups. The outcomes of the painDETECT questionnaire are not established by any sort of psychological questionnaires, nor are there any questions that establish the intensity of pain. Authors suggest that the categorisation of chronic low back pain patients by the painDETECT is independent of these parameters (psychological profiles and pain intensity). They hypothesize that the differences in psychological profiles and pain intensity between the two groups view underlying pain mechanisms identified by the painDETECT.
The underlying pain mechanisms correspond with the concept of neuropathic signs and symptoms of the nervous system. These are the result of maladaptive plasticity of the nervous system and not only the result of lesion or disease of the somatosensory nervous system. Spahr et al. suggest that it is worth considering that maladaptive central nervous system neuropathy is a disease process in itself.
They concluded that these data clarify the differences in clinical profiles of those patients diagnosed with neuropathic low back pain derived from symptom profile assessments rather than from evidence of a lesion or disease process. In addition, their symptoms could be the result of a maladaptive plasticity of the nervous system.
The clinical implications: the painDETECT is a quick and easy to use instrument to differentiate between nociceptive or neuropathic components. Some studies show a high sensitivity (85%) and specificity (80%) and positive predictive accuracy (83%) in low back pain patients. You have to see this instrument as an addition to the physical examination.
To differentiate between nociceptive pain or central sensitization pain the algoritme for 'the classification of central sensitization pain' may probably an useful tool (Nijs et al. 2014). To differentiate between nociceptive pain and neuropathic components, the painDETECT could be a useful tool. All with one purpose: the treatment for the large group of low back pain, more specific to the underlying pain mechanism.
Hester den Bandt, PT, MMT
Manual therapist in Dokkum, Damwoude, Lecturer and PhD-student at Rotterdam University of Applied Sciences in The Netherlands, Institute of Health, Department of Physical Therapy Studies. Member of Pain in Motion International Research Group
2017, Pain in Motion
References and further reading:
Hush, J.M., Stanton, T.R., Siddall, P., Marcuzzi, A., & Attal, N. (2013). Untangling nociceptive, neuropathic and neuroplastic mechanisms underlying the biological domain of back pain. Pain Manage, 3(3), 1-14.
https://www.ncbi.nlm.nih.gov/pubmed/24654765
Freynhagen, R., Baron, R., Gockel, U., & Tolle, T.R. (2006). PainDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Current Medical Ressearch and Opinion. 22, 1911-1920.
https://www.ncbi.nlm.nih.gov/pubmed/17022849
Nijs, J., Torres-Cueco, R., Wilgen van, C.P., Lluch Girbes, E., Struyf, F., Roussel, N., ... Meeus, M. (2014). Applying Modern Pain Neuroscience in Clinical Practice: Criteria for the Classification of Central Sensitization Pain. Pain Physician. 17, 447-457.
https://www.ncbi.nlm.nih.gov/pubmed/25247901
Spahr, N., Hodkinson, D., Jolly, K., Williams, S., Howard, M., Thacker, M. (2017). Distinguishing between nociceptive and neuropathic components in chronic low back pain using behavioural evaluation and sensory examination. Musculoskeletal Science and Practice. 27, 40-48.