In this digital era, healthcare services are more and more evolving towards eHealth applications. Especially for educational and behavioral interventions digital applications are becoming very popular in clinical practice but also in research. If eHealth applications could approximate the level of effectiveness of conventional care, this digital healthcare revolution could imply high cost savings for patients and society. Additionally, access to care would become a lot more convenient for many patients, especially those living in remote areas. This leads us to the question: where is pain neuroscience education (PNE) going in this digital (r)evolution?
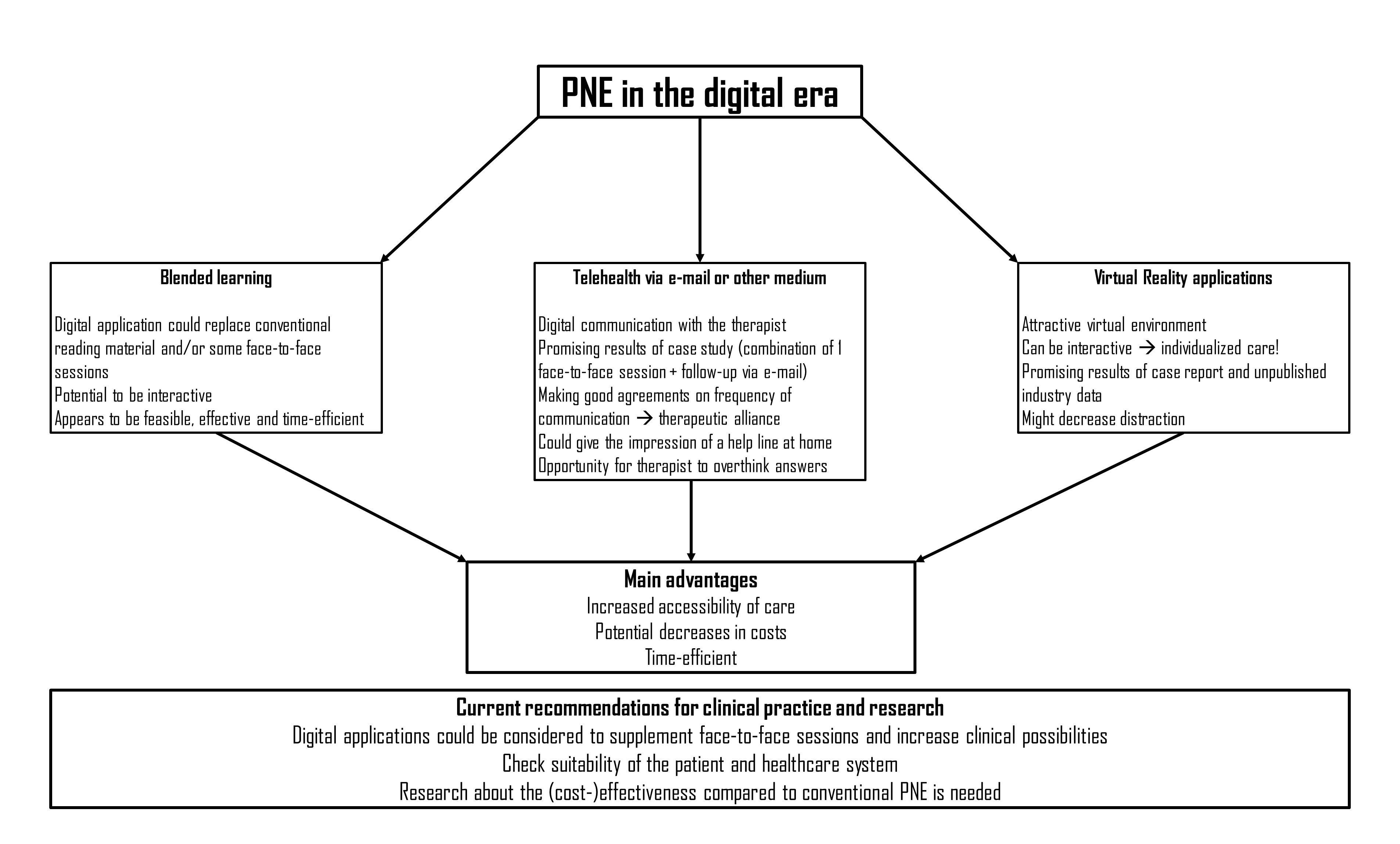
Because the success of PNE is highly depending on the retention of information, it is generally recommended to provide the educational content of PNE in several formats. Moreover because many patients (e.g., patients with chronic pain, perioperative patients or patients with post-cancer pain) are presenting concentration difficulties1,2. The conventional way of accomplishing this multi-format information transfer is by having one or more face-to-face sessions with the patient supplemented by reading material (e.g., educational booklet)2,3.A first step towards digitalizing PNE could be replacing the conventional reading material by a digital and/or online application. Next to replacing for example an educational booklet, this digital module could even replace some of the face-to-face sessions with the therapist as current digital developments ensure the possibility of creating an interactive application, which could even make it individualized. Research by Malfliet et al. (2018) has shown that such a blended-learning approach appears to be feasible, effective and time-efficient4,5, however based on this research we cannot conclude whether blended-learning PNE is better or more cost-efficient compared to a conventional approach. Although not interactive, www.retrainpain.org is already providing online PNE modules for free in different languages which could be used to replace written material in clinical practice. Furthermore, Heathcote et al. (2019) found that quite some PNE video’s (n=106) are available on YouTube6 which could also be used to supplement a PNE intervention. However, the study concluded that only very few of these video’s addressed one or more key concepts of PNE in an engaging manner, and therefore it should be further investigated to what extent these videos could effectively be a worthy supplement of PNE in clinical practice6.
Already a while ago the group of Louw et al. proposed the option of providing PNE and a behavioral follow-up intervention (daily life activity management and exercise therapy) using telehealth by communicating with the patient via e-mail7. Just like the blended-learning approach, this method is still relying on the involvement of a therapist, but implies huge improvements in access to care and decreases of costs for the patient, next to some advantages for the therapist. In their case study they provided one verbal one-on-one session with the patient in clinical practice followed by e-mail follow-up to ensure increased understanding of pain neuroscience and activity management. This approach showed good results for this particular case in terms of pain, disability and fear avoidance beliefs7. When choosing for a telehealth option it should be considered that your contacts are becoming more virtual which could negatively impact therapeutic alliance. This highlights the importance of setting good agreements before initiating telehealth and also complying with these agreements. It should for example be clear what the frequency of e-mail contacts will be and in what amount of time the patient can expect an answer from the therapist. If these agreements are well followed, the patient might even get the impression of having a direct help line at home, which could in turn improve therapeutic alliance.Additionally, consultations via e-mail are providing the therapist with the possibility to overthink his/her answers and to carefully formulate them7.
Last but not least, let’s have a look at the possibilities of Virtual Reality (VR) applications to provide PNE. Research about eHealth VR applications is fast developing, however specifically about PNE, to the best of my knowledge, there is only one case report by Louw et al. (2019)8 available. The latter case was a women suffering from chronic whiplash associated disorder, who received 3 VR sessions containing PNE combined with mindfulness and breathing exercises in clinical practice, but without any involvement of the therapist. The results were promising with clinically important improvements in disability, pain intensity and pain catastrophizing. Furthermore, the patient showed good information retention of the PNE theory and scored her satisfaction with the intervention a 10/10 for each session. The VR PNE intervention in this case report was developed by a firm called BehaVR in cooperation with the group of Adriaan Louw. BehaVR also did an explorative study (unpublished) with the system in 1,880 patients of which they assessed a Global Rating of Change for function and quality of life. Results showed that after the 3th and 6th VR session, over 70% of participants found that their function and/or quality of life improved. This is again a promising result, although we have to look at these results with some criticism as industry data could imply bias due to conflict of interest, and although widely used, it should also be considered that the Global Rating of Change scale is not the most reliable outcome measure as it poorly correlates with functional outcomes and tends to be unreliable over time. Taken together it can be concluded that the possibilities of providing PNE with VR applications look promising, but that definitely more research is needed to evaluate the effectiveness of this digital application compared to conventional PNE provision. Next to the fact that VR applications could again increase the accessibility of care and are nowadays available at a fairly low cost, it is highly suitable for developing interactive applications and bringing the patient into the virtual environment might also decrease distraction.
So can we from now on replace PNE therapists by tablets, laptops and VR goggles? No. I am convinced of the advantages of eHealth applications, especially towards potential cost reductions and increased accessibility of care, and I think that researchers and clinicians should consider such digital applications to supplement and improve their care for certain patients, especially those who live in more remote areas, or have financial or transport difficulties. However, up until now, I am also still convinced of the added value of a therapist of flesh and blood, with whom patients can build a strong therapeutic alliance, and this because of several reasons. First of all, more research is needed about the effectiveness of digital applications for providing VR, and it has to be explored how to make these interventions highly interactive so they can provide PNE in an individualized manner, which is one of the key principles of high-quality PNE interventions. Second, we have to consider that at this moment not everyone is ready for digital applications, the older generation of today might still prefer an educational booklet over an app for example. Third, recent research has shown that so far the most optimal format for using digital applications for behavioral interventions is by combining them with some form of therapist counselling9,10, meaning that the therapist still has an important role to play. Last, it should be mentioned that in many healthcare systems nowadays, there is still no healthcare nomenclature for digital applications as proposed here available, meaning that often also because of administrative reasons there should still be face-to-face, and even hands-on, contacts between the therapist and patient.
Eva Huysmans
2019Pain in Motion
References and further reading:
1. Meeus M, Nijs J. Central sensitization: a biopsychosocial explanation for chronic widespread pain in patients with fibromyalgia and chronic fatigue syndrome. Clin Rheumatol 2007; 26(4): 465-73.
2. Nijs J, Paul van Wilgen C, Van Oosterwijck J, van Ittersum M, Meeus M. How to explain central sensitization to patients with 'unexplained' chronic musculoskeletal pain: practice guidelines. Man Ther 2011; 16(5): 413-8.
3. Louw A, Butler DS, Diener I, Puentedura EJ. Development of a preoperative neuroscience educational program for patients with lumbar radiculopathy. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists 2013; 92(5): 446-52.
4. Malfliet A, Kregel J, Meeus M, et al. Blended Learning Pain Neuroscience Education for People With Chronic Spinal Pain: Randomized Controlled Multicenter Trial. Phys Ther 2018; 98(5): 357-68.
5. Malfliet A, Kregel J, Coppieters I, et al. Effect of Pain Neuroscience Education Combined With Cognition-Targeted Motor Control Training on Chronic Spinal Pain: A Randomized Clinical Trial. JAMA neurology 2018; 75(7): 808-17.
6. Heathcote LC, Pate JW, Park AL, et al. Pain neuroscience education on YouTube. PeerJ 2019; 7: e6603-e.
7. Louw A. Therapeutic neuroscience education via e-mail: a case report. Physiotherapy theory and practice 2014; 30(8): 588-96.
8. Louw A, Louw C, Flynn T. Case Report: Pain Neuroscience Education Using Virtual Reality. Journal of Physiotherapy Pain Association 2019; (46): 4-7.
9. Joiner KL, Nam S, Whittemore R. Lifestyle interventions based on the diabetes prevention program delivered via eHealth: A systematic review and meta-analysis. Prev Med 2017; 100: 194-207.
10. Hurkmans E, Matthys C, Bogaerts A, Scheys L, Devloo K, Seghers J. Face-to-Face Versus Mobile Versus Blended Weight Loss Program: Randomized Clinical Trial. JMIR Mhealth Uhealth 2018; 6(1): e14-e.