Over the past decades (and earlier published blogposts: http://www.paininmotion.be/blog/detail/mechanism-b... and http://www.paininmotion.be/blog/detail/pain-mechan...), a mechanism-based approach to pain management has been progressively underlined to achieve clinically meaningful improvements in pain outcomes. Identification of patient symptoms and the relation with underlying pathophysiological mechanisms is essential to enhance prevention and treatment of these symptoms. For various patient populations, recommendations have been published for classification regarding the pathophysiological mechanisms of pain based on the clinical diagnosis. However, Cruz-Almeida et al. (2014) stated that the clinical diagnosis typically provides limited information on the pathophysiological mechanisms underlying the pain experience that may guide the choice of treatment. A promising method for investigating pathophysiological mechanisms that contribute to the development and/or maintenance of pain is quantitative sensory testing (QST).
QST is an umbrella term for non-invasive assessment techniques evaluating the functioning of the somatosensory nervous system. This somatosensory system is a sensory system that includes peripheral receptors and central processing systems (e.g. the spinal cord, the brain, etc.) and allows the human body to perceive the physical sensations of pressure, temperature, and pain. Through QST, the different qualities of the somatosensory system can be tested separately by administering standardized objective stimuli, such as thermal or mechanical stimuli, and quantifying the self-reported sensory experience (Hall 2015). Accordingly, QST will evaluate the function of small afferent unmyelinated C fibers, myelinated A-alpha, A-beta and A-delta nerve fibers, as well as corresponding central pathways. QST may provide more information on the neuronal pathways underlying a somatosensory dysfunction, although it cannot provide information on the precise cause of somatosensory dysfunction. It is also worth noting that, in addition to methodological (e.g. test instructions) and environmental influences (e.g. noise), the reaction of the patient to the test stimulus (and thus the QST-result) may be affected by psychosocial factors. This makes QST a psychophysical evaluation method rather than a completely objective assessment of sensation and pain (Backonja 2013, Hall 2015).
Multiple QST methodologies have been described in literature to comprehensively evaluate functioning of the somatosensory system. Standardization of QST is recommended but not self-evident. The German research network on neuropathic pain (Deutschen Forschungsverbundes Neuropathischer Schmerz, DFNS) implemented a standardized QST protocol to evaluate somatosensory functioning, in order to standardize QST in research and clinical practice (Mucke 2016).
Most often, QST is used in terms of threshold detection: tests to determine the detection threshold of a stimulus (i.e. the lowest stimulus magnitude that a person can experience) and the pain threshold of a stimulus (i.e. the lowest stimulus magnitude that a person experiences as painful/unpleasant). These threshold values are examined by administering a stimulus of increasing or decreasing magnitude to the patient. Most frequently described stimulus modalities are thermal (e.g. heat, cold) or mechanical (e.g. tactile, pressure, vibration) stimuli.
In clinical practice, stimulation with simple equipment such as a toothpick, cotton wool or metal coins can be used to assess the according somatosensory pathway. Sensory loss and/or gain of function can be evaluated by comparing findings with the contralateral side. Standardization and quantification of this clinical sensory testing is rather difficult (Backonja 2013). However, for improving the prevention and management of pain and sensory deficits in clinical practice, it is very important to use this qualitative variant of QST, rather than no sensory testing at all (Beales 2021).
Besides methods to evaluate local sensory detection or pain (i.e. primary hyperalgesia), QST is also used to evaluate the endogenous pain processing system of pain inhibition and facilitation, which are more centrally mediated neural processes (Backonja 2013). This can be achieved by assessing the tolerance for pain in a more distant region of the affected body region (i.e. secondary hyperalgesia) for example at the level of the hand or lower leg. In addition, the process of pain inhibition can be assessed specifically based on the response to the simultaneous administration of multiple pain stimuli (i.e. conditioned pain modulation) (Yarnitsky 2010). In case of a normal functioning endogenous pain-inhibiting system, the second pain stimulus would be experienced as less painful than during administration of only one pain stimulus (i.e. pain inhibits pain principle). When an increase in pain intensity is reported with administration of multiple pain stimuli together, the endogenous pain-inhibiting system is considered as dysfunctional. Furthermore, the process of pain facilitation can also be evaluated based on the response to the repetitive application of a (pain) stimulus (i.e. wind-up or temporal summation) (Mucke 2016). Pain facilitation is considered when the pain experience increases during repetitive application with a (painful) stimulus and/or this pain experience manifests after the final stimulation.
Lack of information on the therapeutic usefulness, insufficient understanding of application requirements and/or fear for time-consuming test procedures may contribute to the reluctance to integrate QST procedures into standard clinical practice. The purpose of this post was to provide more background to what QST actually includes and how it can be applied in research and clinical practice. QST may help to understand the pain processes underlying the clinical presentation of a patient and it can be easily integrated in the assessment and treatment for acute as well as chronic pain problems.
Lore Dams
Physiotherapist and PhD Researcher at University of Antwerp and KU Leuven. Her research focuses on rehabilitation during and after breast cancer treatment, with a particular interest in sensory disturbances and pain.
2021 Pain in Motion
References and further reading:
Cruz-Almeida Y, Fillingim RB. Can quantitative sensory testing move us closer to mechanism-based pain management? Pain Medicine. 2014;15(1):61-72
Backonja MM, Attal N, Baron R, et al. Value of quantitative sensory testing in neurological and pain disorders: NeuPSIG consensus. Pain. 2013;154(9):1807-19.
Beales D, Mitchell T, Moloney N, Rabey M, Ng W, Rebbeck T. Masterclass: A pragmatic approach to pain sensitivity in people with musculoskeletal disorders and implications for clinical management for musculoskeletal clinicians. Musculoskelet Sci Pract. 2021 Feb; 51:102221.Epub 2020 Jul 18.
Hall T, Briffa K, Schafer A, Tampin B, Moloney N. Quantitative Sensory Testing: Implications for clinical practice. In: Jull G, Moore A, Falla D, Lewis, J, McCarthy C, Sterling M, editors. Grieve's Modern Musculoskeletal Physiotherapy. 4th edition. UK: Elsevier Health Sciences; 2015. p. 194-201.
Mucke M, Cuhls H, Radbruch L, et al. Quantitative sensory testing (QST). English version. Schmerz. 2016.
Rolke R, Baron R, Maier C, et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain. 2006;123(3):231-43.
Starkweather AR, Heineman A, Storey S, et al. Methods to measure peripheral and central sensitization using quantitative sensory testing: A focus on individuals with low back pain. Applied Nursing Research. 2016;29:237-41.
Yarnitsky D, Arendt-Nielsen L, Bouhassira D, et al. Recommendations on terminology and practice of psychophysical DNIC testing. European Journal of Pain. 2010;14(4):339.
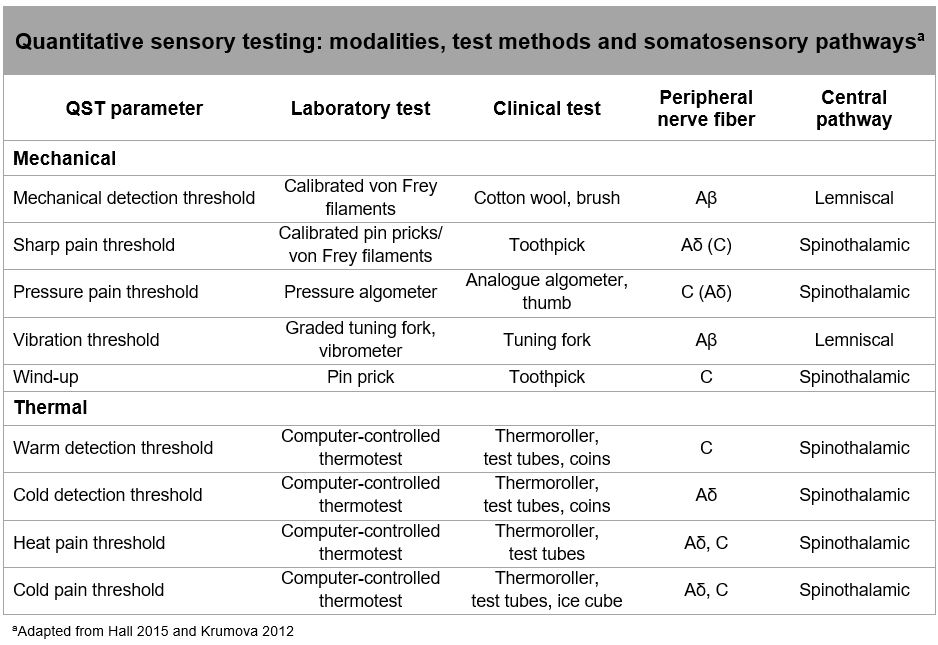
Table
Krumova EK, Geber C, Westermann A, et al. Neuropathic pain: is quantitative sensory testing helpful? Current Diabetes Reports 2012;12(4):393–402.
Hall T, Briffa K, Schafer A, Tampin B, Moloney N. Quantitative Sensory Testing: Implications for clinical practice. In: Jull G, Moore A, Falla D, Lewis, J, McCarthy C, Sterling M, editors. Grieve's Modern Musculoskeletal Physiotherapy. 4th edition. UK: Elsevier Health Sciences; 2015. p. 194-201.